Kessen/Kerwin Oral Boards
Case 1. Adult male with neutropenia due to chemotherapy presents with abdominal pain and sepsis picture. Diagnosis was typhlitis, otherwise known as neutropenic enterocolitis. There is compromised integrity of bowel wall that leads to sepsis. Treatment is hemodynamic support and big gun antibiotics.
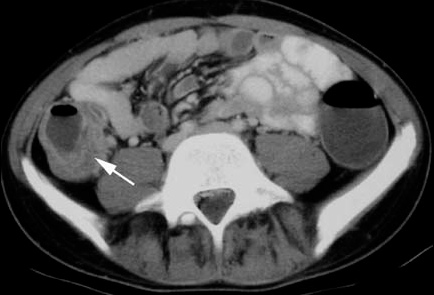
Typhlitis
Case2. Pt receiving chemotherapy for lung cancer. Pt had a seizure. Labs showed an acute increase in Creatinine, hyperkalemia, hyperphosphatemia, hyperuricemia, and severe hypocalcemia. Dx was Tumor Lysis syndrome. Management is hydration, manage hyperkalemia, give calcium. Be cautious with bicarb because it can increase precipitation of calcium. Rasburicase is a medication that can lower uric acid levels. Kerwin states this is the money drug for Tumor Lysis Syndrome.
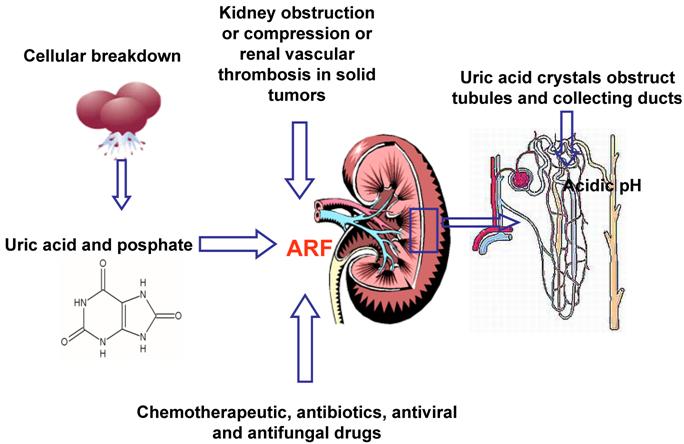
Tumor Lysis Syndrome
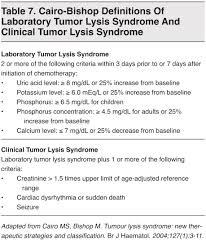
Tumor Lysis Syndrome
Case3. 72yo male presents with dyspnea. 90/65 T=37.2 HR=116 R=25 Glucose=90 Cachectic. Hx of COPD and mesothelioma. Ultrasound showed pericardial effusion. EKG showed electrical alternans. Pt had malignant pericardial effusion causing tamponade. Pericardiocentesis was performed with improvement in clinical condition.
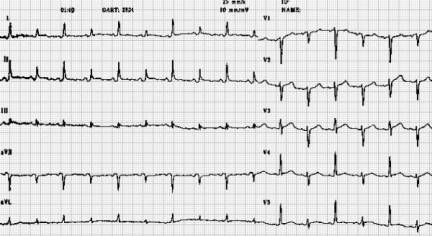
Electrical Alternans
Elise comment: Great set of cancer related oral board cases. There is a really nice reinforcement of the management of cancer emergencies on a recent EM Rap.
McGurk Billing and Coding
Cindy Chan comment: You have to be careful with template charting to make sure there aren’t unintended findings automatically listed on the chart. McGurk response: We have seen charts in which elderly female patients were noted on ROS to deny scrotal edema. Felder comment: We have seen stroke case charts with ROS for neuro listed as negative. So be careful with template charting.
The line “reviewed as documented in chart” is not helpful for billing without a date listed as to what date of records were reviewed. Harwood comment: We need to change the template to say “reviewed as documented in patient summary screen”.
For an EM level 5 you need PMH/Surg HX and either past social hx or family hx. You don’t need both social and family hx. Harwood comment: Just ask/document No asthma, lives with parents or HTN and smoker. McGurk comment: Lives independently, lives in a NH, assisted care are all usable comments for social hx.
There is typically a 5 day lag between when you see the patient and when the coders get to the chart. Get you charts done and signed within 5 days. Girzadas comment: Get your charts done in less than 5 days. There’s an old Joe Wood comment, “The longer you take to finish your charts the more it starts to look like fiction.”
Chan Stroke Core Measures
The important core measures for stroke in the ED are:
- Thrombolytic therapy given when appropriate,
- Patients with afib/aflutter receive anticoagulation therapy,
- ASA or other anti-thrombotic therapy by day 2.
Harwood comment: Many times there may be concerns by neurology about starting heparin in the ED. So giving heparin in the ED for afib and stroke may not be indicated in many cases. Possibly documenting in the chart the contraindication or relative contraindication for heparin may help meet the core measure.
Beckmeyer Safety Lecture Improving the Care and Safety of Patients Boarding in the ED
Strategies to improve the care/safety of boarding ED patients:
Increasing face to face communication in the ED between ED physicians and Intensivists
Ask intensivists to round in the ED in the AM
Bedside rounding
At sign out be sure antibiotics/meds/labs are ordered
Improved order sets for boarding patients
Push back on soft ICU admits and try to admit to step down or tele
Downgrade patients to floor admits whenever possible
Use the SVTU or SINI as an area to overflow patients
Tranfer to outside ICU?
Urumov/Harwood comment: Transfer to outside hospital ICU can be done but has risks and negative poltical/financial consequences. It can be done on a case by case basis for ICU players that are stabilized and not requiring super high level of care like 3 pressors. C.Kulstad comment: Be really careful about transferring out ICU players. You are not transferring to a higher level of care. It is really the same level of care so if patient crumps in route you are responsible for that decision.
5W step down is basically an ICU without resident coverage. C. Kulstad comment: 5W doesn’t have the same nursing staffing as does an ICU. Staffing ratio is 3:1 on 5W. SVTU is SINI overflow with no resident coverage.
ACMC clinical tools on the web has a parenteral administration guide. It will tell you what drips can be managed on what unit.
DKA must go to an ICU. Non-DKA on an insulin drip can go to any unit. Maletich comment: Endocrine consults can help with getting access to non-ICU settings for non-DKA patients.
The SSU can take 1-2 ICU level patients. Maletich comment: May be a good unit to put a head injury patient with a minor finding on CT head who needs observation.
Remember to report errors/near misses. Go to Advocate homepage>> culture of safety >> safety event reports forms.
For unattached ICU admits, the admitting/attending physician should be the on-call Intensivist. The Adult Medicine Attending on call should not be listed at all for ICU admits.
Suter AAEM Guest Speaker, Pediatric Trauma “Why Kids are Different”
From a physiologic stand point, kids under 8 years of age are different than adults. 8 years of age seems to be the cut off that really differentiates kids from adults from a physiology perspective. Kids over 13 are really like little adults.
Physiological differences in kids: Force is distributed to a smaller area. Greater relative body surface area results in greater heat loss. Smaller and more anterior airway. Greater airway resistence in kids. Relatively larger head to body ratio. More flexion and extension ligamentous injuries due to head size. Organs are more anterior and less protected making them more vulnerable. Greater capacity to compensate for shock. Salter harris fractures. More sensitive to radiation. Infants are nose breathers.
During intubation of young child, don’t put pad behind head. It puts the neck in flexion and limits airway visibility. Miller (straight) blade is preferred in kids. Atropine is indicated in kids less than 8 to prevent bradycardia during intubation.
Pulse is a more reliable guide to cardiovascular instability than BP due to kids’ ability to compensate for volume loss.
Don’t be hesitant to place an IO line in patients with difficult venous access.
Leading cause of death is head injury, but 90% of head injuries are minor.

Glascow Coma Score for Kids
C. Kulstad sent out the PECARN Head injury Rules to everyone. This is a synopsis image.
Cspine injuries in kids <8yo are more likely to be high cervical injuries above C3.

Pseudosubluxation
Kids with head/neck injury that have paresthesias in the extremities and have negative c-spine films. They need an MRI to rule out SCIWORA.
Harwood question: At what age cutoff do you need to start worrying about aortic injury due to deceleration injury? Response: somewhere around 8yo. Harwood comment: I was thinking somewhere around 12yo. Both agreed literature was scant on this issue.
FAST exam is not as reliable in kids than in adults. Lam comment: I still feel FAST has utility to identify serious injury in the injured child. Response: Agree, just remember if no abnormality is identified it doesn’t mean there is no injury.
Transfer decisions to Trauma Center can be aided by Pediatric Trauma Score. Score less than 8 indicates need for transfer to Trauma Center.
Elise comments: "Cuffed Versus Uncuffed Endotracheal Tubes
Both cuffed and uncuffed endotracheal tubes are acceptable for intubating infants and children (Class IIa, LOE C). In the operating room, cuffed endotracheal tubes are associated with a higher likelihood of correct selection of tube size, thus achieving a lower reintubation rate with no increased risk of perioperative complications.88,–,90 In intensive care settings the risk of complications in infants and in children is no greater with cuffed tubes than with noncuffed tubes.91,–,93 Cuffed endotracheal tubes may decrease the risk of aspiration.94 If cuffed endotracheal tubes are used, cuff inflating pressure should be monitored and limited according to manufacturer's instruction (usually less than 20 to 25 cm H2O).
In certain circumstances (eg, poor lung compliance, high airway resistance, or a large glottic air leak) a cuffed endotracheal tube may be preferable to an uncuffed tube, provided that attention is paid to endotracheal tube size, position, and cuff inflation pressure (Class IIa, LOE B)."
Harwood comments: Here's the Peds blunt trauma rules. PECARN no longer recommends that finding 20 RBC's in urine mandates CT abdomen/pelvis.
Ann Emerg Med. 2013 Aug;62(2):107-116.e2. doi: 10.1016/j.annemergmed.2012.11.009. Epub 2013 Feb 1.
Identifying children at very low risk of clinically important blunt abdominal injuries.
Holmes JF, Lillis K, Monroe D, Borgialli D, Kerrey BT, Mahajan P, Adelgais K, Ellison AM, Yen K, Atabaki S, Menaker J, Bonsu B, Quayle KS, Garcia M, Rogers A, Blumberg S, Lee L, Tunik M, Kooistra J, Kwok M, Cook LJ, Dean JM, Sokolove PE, Wisner DH, Ehrlich P, Cooper A, Dayan PS, Wootton-Gorges S,Kuppermann N; Pediatric Emergency Care Applied Research Network (PECARN).
Source
Department Emergency Medicine, UC Davis School of Medicine, Sacramento, CA, USA. jfholmes@ucdavis.edu
Abstract
STUDY OBJECTIVE:
We derive a prediction rule to identify children at very low risk for intra-abdominal injuries undergoing acute intervention and for whom computed tomography (CT) could be obviated.
METHODS:
We prospectively enrolled children with blunt torso trauma in 20 emergency departments. We used binary recursive partitioning to create a prediction rule to identify children at very low risk of intra-abdominal injuries undergoing acute intervention (therapeutic laparotomy, angiographic embolization, blood transfusion for abdominal hemorrhage, or intravenous fluid for ≥2 nights for pancreatic/gastrointestinal injuries). We considered only historical and physical examination variables with acceptable interrater reliability.
RESULTS:
We enrolled 12,044 children with a median age of 11.1 years (interquartile range 5.8, 15.1 years). Of the 761 (6.3%) children with intra-abdominal injuries, 203 (26.7%) received acute interventions. The prediction rule consisted of (in descending order of importance) no evidence of abdominal wall trauma or seat belt sign, Glasgow Coma Scale score greater than 13, no abdominal tenderness, no evidence of thoracic wall trauma, no complaints of abdominal pain, no decreased breath sounds, and no vomiting. The rule had a negative predictive value of 5,028 of 5,034 (99.9%; 95% confidence interval [CI] 99.7% to 100%), sensitivity of 197 of 203 (97%; 95% CI 94% to 99%), specificity of 5,028 of 11,841 (42.5%; 95% CI 41.6% to 43.4%), and negative likelihood ratio of 0.07 (95% CI 0.03 to 0.15).
CONCLUSION:
A prediction rule consisting of 7 patient history and physical examination findings, and without laboratory or ultrasonographic information, identifies children with blunt torso trauma who are at very low risk for intra-abdominal injury undergoing acute intervention. These findings require external validation before implementation.
There was a discussion about Cspine CT vs Plain films in injured kids.
Trale Permar comment: CT Cspine is more sensitive in kids. See graph below

Think about Tumor Lysis syndrome in patients with blood cancers and soon after initiation of cancer treatment. Big red flag is acute worsening of renal function in patient recently started on chemotherapy. If you don't think to check uric acid and phosphate levels, you can easily fixate on the hyperkalemia and miss the underlying diagnosis. DON'T give calcium in asymptomatic patient as you can cause CaPO4 deposition and make the patient worse. If they have neuroirritability, you may have to give some calcium, but good idea to call nephrology and work with their recommendations.
