McDermott Study Guide ENT/Dental
Never re-implant avulsed primary teeth.
With cribiform plate fractures you have to be alert for CSF leak. Beta 2 Transferrin is a more specific test for CSF fluid than measuring glucose from fluid draining from the ear or nose. The residents (Htet and Kennedy) said in the SINI they run a Beta2 Transferrin test on fluid from the nose or ear or even from a swab of the nose or ear to check for CSF leak.
The most common bacterial causes of parotitis or sialoadenitis is staph, strep, and anaerobes. In nursing home patients you have to use vancomycin to cover MRSA.
Adult epiglottitis usually presents with sore throat and difficulty swallowing. Adult patients don’t usually present with stridor/drooling.
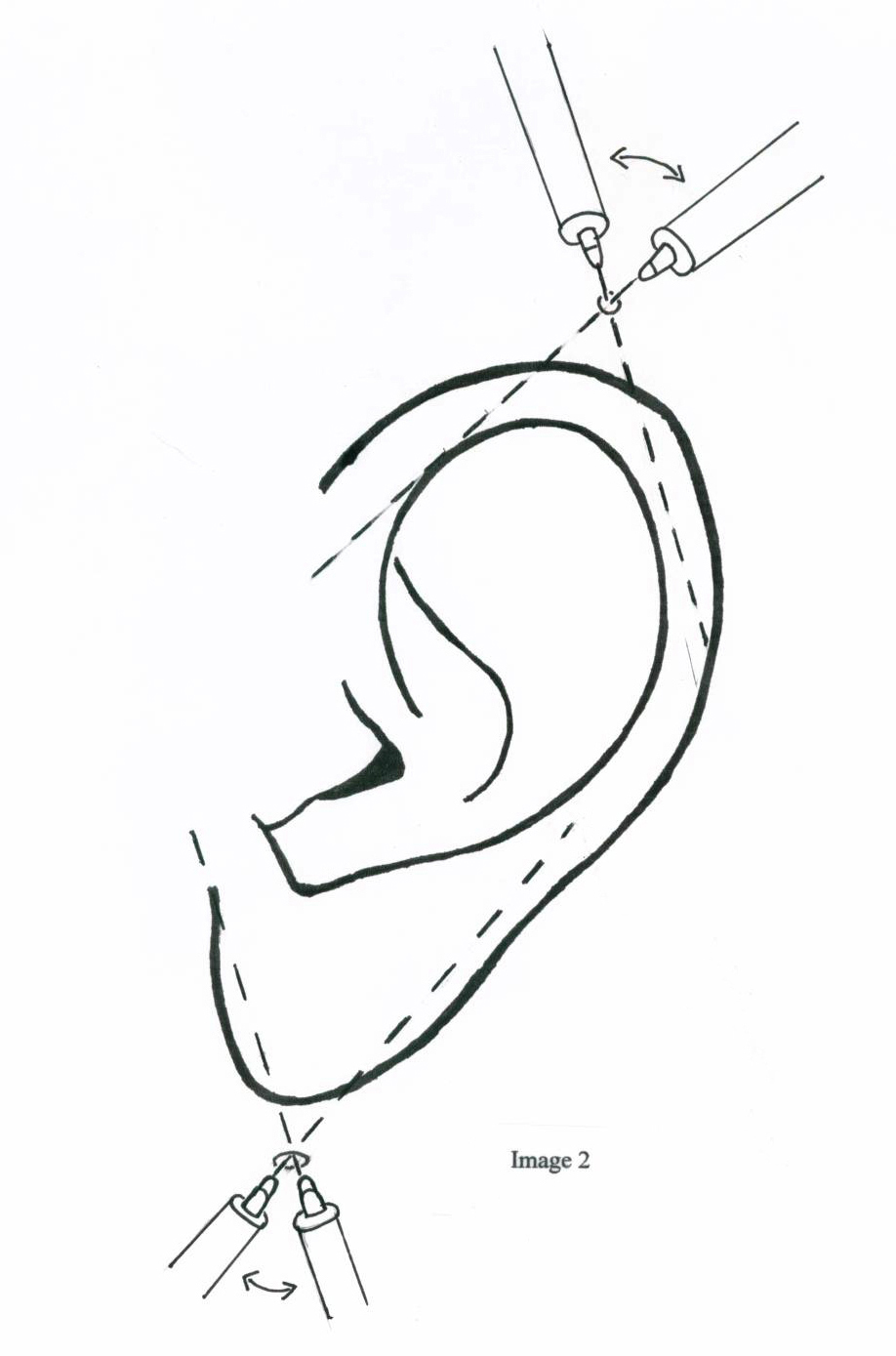
To fully nerve block the ear you should place an auriculotemporal nerve block.
Elise comment: This block works very well for complex ear lacerations. Patients get great anesthesia from these blocks.
*Auriculotemporal nerve block
Management of optic neuritis requires IV steroids. IV steroids improve the time to improvement, have less recurrances of optic neuritis and may prevent the development of MS. IV steroids do not improve visual outcome over oral steroids.
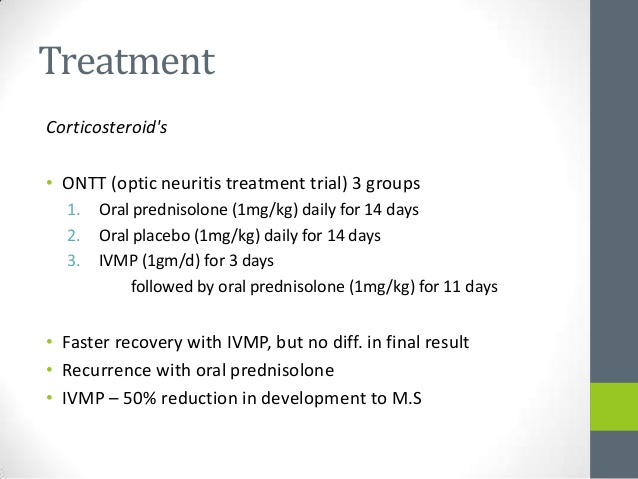
*Outcomes of IV vs Oral Steroid Trial in Optic Neuritis
Risk factors of posterior nasal packing include cardiac arrest, hypoxia, and necrosis of the colunmella, Use only as much pressure in the balloons as needed. All patients with posterior balloon packing need to be admitted.
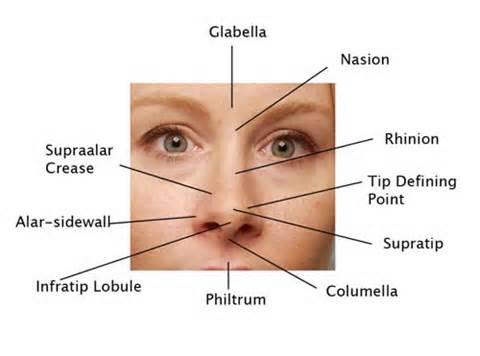
*Nasal anatomy including columella and philtrum
Ear drops to use when you have a concern for a perforated tm: Use cortisporin otic suspension . Floxin otic solution is another option and is the only FDA approved ear drop for use with perforated TM. Don’t use any other otic solutions when concerned about a perforated TM because solutions have lower ph’s than suspensions. “Otic solution is not the solution”. Alternatively, you can use ophthalmic preparations of a flouroquinalone. They are less irritating than otic preparations and in general cheaper.
Ludwigs’s angina most commonly develops from an infection of the lower molar.
Final Jeapordy Question: Genu 7 Bell’s Palsy is a stroke that looks like Bell’s Palsy but the patient cannot abduct the ipsilateral eye. Stroke is in the pons.
Katiyar Critical Care Billing and Coding
Critical care codes have higher RVU’s than other EM codes.
Medicare pays $35.80 per RVU.
A fast track patient generates about $62 in physician reimbursement. A Cardiac patient generates $175. A Critical Care patient generates $225 in physician reimbursement.
Definition of critical care: high probability of sudden, clinically significant, or life threatening deterioration requiring the highest level of physician attention.
Simple test of critical care: Does this patient have an illness/injury that if you do nothing, they could die? If the answer is yes, then it is likely critical care.
- Some examples of critical care: Being called to the bedside to evaluate opiate overdose with shallow breathing.
- New onset seizure with fever in a patient with multiple other medications and medical problems.
- Evaluation of acute hypotension of any cause.
- Supraventricular tachycardia requiring Adenosine intervention.
- Admission for acute renal failure with critical hyperkalemia being managed with or with acute dialysis.
- Admission for symptomatic hyponatremia requiring 3% NaCl.
- Admission for pneumonia or COPD exacerbation requiring BiPAP therapy.
- Admission for large volume gastrointestinal bleeding with tachycardia.
- Admission for severe DKA requiring an insulin drip.
- Admission for symptomatic hypertension with headache or chest pain on medication infusion therapy.
- Admission for rapid atrial fibrillation on continuous Amiodarone infusion.
- Being called to the bedside to evaluate chest pain with new ST elevation EKG changes.
- NSTEMI Patient
- Being called to the bedside to evaluate a patient with acute stroke signs and symptoms.
There are some diagnoses that you can bill critical care and still discharge the patient: overdose, anaphylaxis, angioedema, asthma exacerbation. Be careful of billing critical care with a discharge. It could trigger an audit. A medicare audit is bad news and it covers the last 4 years not just the chart that triggered the audit!
ICU admission is not a requirement for critical care billing. For example, patients with severe asthma or CHF can be significantly improved by aggressive care in the ED and then be admitted to tele or the floor. These patients still qualify for critical care billing.
In addition to documenting the time you spent, you need a macro stating something to the effect of “Due to the patients unstable presentation, he required my immediate attention and intervention for 35 minutes Also document your repeat exams and how the patient was progressing, the interventions you made, and how the patient was responding to treatment.
You cannot bill critical care on a failed resuscitation.
If you are working with a resident, the time you billed critical care has to be your time and not include the resident’s time. Time spent teaching cannot be counted as critical care. The same general rules apply if you are working with a midlevel provider.
Critical care time includes documentation time, interpretation of testing, review of prior records, bedside care, re-assessment, discussion with family, and discussion with other physicians.
The time you document as total critical care time is a conservative estimate of the total time you spent managing the critically ill patient. You don’t need to break down the total time you spent in itemized fashion in your note. You can do that (5 minutes interpreting ABG, 10 minutes discussion management decisions with patient’s family, 20 minutes at besdside managing hemodynamic instability) but it is not necessary.
Be very careful to not overbill critical care. The standard percentage of critical care charts for an EM doc is less than 5%. On most shifts you can probably bill critical care for one or two patients. If you are billing critical care over 5%, you are at risk for an audit.
Kalimullah Critical Care Fellowship Training and Employment
Ejaaz went over the various training routes to becoming a board certified critical care physician.
The IM route has the benefit of learning to manage many complex, multiply co-morbid patients. The majority of practicing intensivists are IM trained so politically this track may give you more job opportunities. The downside is you need 6 months of IM experience, 3 months of which have to be in the ICU prior to supervising IM residents. That is an RRC requirement for IM training programs. So you need to do a lot of MICU in residency or at the beginning of fellowship. The number of EM trained fellows is limited to 25% of total fellow complement in each IM Critical Care program .
The Anesthesia Critical Care route has the benefit of a common application form and a match. The curriculum is more tolerant of EM residents. You don’t have all the IM prerequisites. You only need 4 months of critical care training during residency. Anesthesia has a resuscitation-centric philosophy. There is common interest between EM and Anesthesia with airway management. You can get TEE training in this track. You will get a broad clinical exposure including extensive surgical subspecialty exposure. The downsides are less time spent in the MICU and less exposure to ID/nephrology/pulmonary/cards. You frequently have to co-manage your patients with the surgeon.
There are only 17 programs nationwide that are set up to take an EM resident as a fellow. Not a lot of spots for EM grads. Anesthesia grads have shown increasing interest in these spots so there is significant competition.
Surgical Critical Care Route. Up sides: A lot of experience in trauma and acute surgical illness. You will likely take care of patients with less co-morbidities than in an MICU. It can be a springboard for a career in a surgical ICU. Downsides: Only 6 programs nationwide are set up for EM grads. The first year of the curriculum is a “supplemental educational program in surgery for emergency physicians”. This year is basically a year of surgical residency EM residents are largely taken outside the match. You will be co-managing patients with surgeons. Less job opportunities after fellowship because many community hospitals don’t have SICU’s or surgical subspecialty ICU’s.
Employment for EM critical care fellowship trained physicians: 49% do both EM and critical care practice. 25% do critical care only. 21% do EM only. 63% work in academic centers. If a doc does both EM and critical care in his practice, they tend to work more days than a doc who does only one or the other. There is something called Crippen’s Law. This states that by 5 years all dual trained EM/Critical care docs will be practicing 100% in either EM or Critical Care but not both. This frequently turns out to be the case.
Bolton Duty and Ethical Dilemma
4 principals of ethics : Autonomy, beneficience (work to benefit the patient), nonmaleficence (do not harm) and justice (distribute resources fairly).
Rapid decision tool for ethical questions:
Is there already a standing rule for this situation? If yes, follow the rule. If no then,
Can you buy time? If yes buy time with medical stabilization. If no then
be impartial, follow the golden rule. Your decision should be universalizable. It should be able to be applied in the same way tomorrow to another patient. Finally, you should be able to explain and justify the decision to a lay person. If you your decision does not follow the golden rule, is not fit to be applied in all situations, or you feel like you can’t justify it to your mom, you should probably rethink your decision.
Case: 16yo female is found to be pregnant and doesn’t want her mom told. Your response to this request for confidentiality depends on your determination as to whether the patient has capacity to make this decision. Ask the patient why she doesn’t want this information divulged. Try to convince the patient to divulge the information to her mom. If the patient won’t speak to her mom about her pregnancy, then you have to decide if she has capacity to understand the ramifications of her decision. If you think she does have capacitythan confidentiality is indicated. If you think she does not have adequate capacity, then you need to divulge the pregnancy test result with the patient’s mom and document why you did not feel the patient had capacity to make the decision she did.
Case: Patient with metastatic cancer. Patient is peri-arrest. Patient has signed DNR. Family in the ED says do everything. The issues here are futility and nonmaleficence. What the family wants is contrary to the patient’s wishes. Ask the family why they want the patient to be resuscitated. The family said that another family member was coming to the hospital and they would want her alive until he got there.
There was a animated discussion about whether to intubate the patient to keep her alive until the son arrived. There was pretty much 50:50 split in the group between those who would or would not. Ejaaz’s comments: Autonomy is the most valued ethical principal in the US. You have no obligation to give futile care. Some patients will have PTSD after ICU care despite heavy sedation. So sedation while the patient is intubated is not sure to prevent suffering. Finally there is a slippery slope of having to provide further care beyond intubation to keep the patient alive for those 6 hours. Discuss with the family that there is a conflict between the patient’s comfort and their desire to keep her alive. Tell the family that they will have to pick which outcome(prolonged life with some possible suffering vs death with no suffering) they think the patient would value more. Braden Parker comment: There is also a justice component in this case in which this patient is receiving futile care in the ICU that is keeping another patient out of the ICU.
Ebola issues: Do we as physicians have a duty to take care of an ebola patient? Because we are a profession we have a responsibility to care for these patients. The AMA made a statement in 1983 that physicians have to take care of AIDS patients. There are some situtions that may take away this responsibility: physicians who are pregnant moms or single parents. We are not responsible to care for patients without adequate preparation and protection. However, if there are proper safeguards and protection and knowledge of the disease we have an obligation to care for the disease. Futility is a factor as well. There is agreement that we will not intubate or code ebola patients. Elise comment: It was not a positive time for medicine when in the 1980’s some physicians were refusing to care for AIDS patients.
17yo female with non-hodgkin’s lymphoma. The patient refused chemotherapy. Chemotherapy for this disease has an 80% success rate. The patient’s mom supported her daughter’s decision. A Court forced the teen to undergo chemotherapy. There was a animated discussion over whether it was appropriate to force the patient to receive chemotherapy over the patient’s and the mom’s desires.