Htet/Meyers STEMI Conference
Case 1. Patient with chest pain.
*Initial EKG
Cardiologist comments: It is unusual to have isolated V1 and V2 ST elevation without ST elevation in the other precordial leads. If the ST elevation in V1 And V2 is related to proximal LAD occlusion it should also affect the other leads. EKG also shows IRBB and RV strain. It is also unusual for a STEMI to be bradycardic if it is not an inferior STEMI.
It was learned that patient had history of chronic aortic dissection and prior PE. Patient was taken to the cath lab and a Type A aortic dissection was identified.
There was discussion of the risk of double dye load for CTA followed by coronary angiogram. Dr. Silverman said that even if you take the patient to cath first without CT chest, the patient would still get about the same dye load for an aortic root shot followed by evaluation of the coronary arteries. An alternative approach could be TEE for a patient with an elevated creatinine.
Dr. Silverman noted that pain from aortic dissection is more abrupt then that for AMI.
There was a discussion about the use of d-dimer to evaluate for aortic dissection. Cardiology faculty was relatively pro d-dimer for this indication. EM faculty was more cautious about d-dimer in this setting. Harwood and Elise felt d-dimer will miss about 5% of aortic dissections. Al-Kaled stated that if an elisa d-dimer is negative the patient does not have a dissection. Drs. Harwood, C. Kulstad and Lovell almost had dissections of their own in response to this statement. They felt the data shows that D-dimer can miss intramural hematomas/dissections. Clearly this issue is controversial.
IRAD data on Aortic dissection shows that “classic” history and physical findings are not commonly present.
Elise comments and data: To be "low risk", you need a score of zero, meaning none of these features. The patients I'm considering dissection in are usually patients who have abrupt, ripping, tearing pain, and therefore will not be "low risk". Lower end of likelihood ratio 96%. As Harwood said, not a disease to accept a 4% miss rate, and with the additional issue of low specificity, I'm not a fan of using d-dimer for diagnosing aortic dissection.
*Aortic Dissection Decision Rule
Cardiology comment: If patient has a pericardial effusion on echo in the setting of chest pain think aortic dissection.
Consensus by cardiology: Do a CTA if you consider aortic dissection.
Case 2. Chest pain in a patient with recent stroke.
EKG
If you see a heart rate of 150 consider A-flutter. If you see an RSR pattern in addition to a heart rate of 150 that makes A-flutter even more likely.
CXR shows very prominent right pulmonary artery. Bedside US showed dilated RV. CTPE done and showed PE.
2.Massive vs. Sub-Massive PE
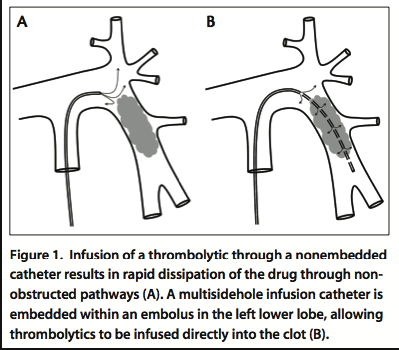
EKOS catheter was placed in pulmonary artery and TPA was given over 12 hours.
* EKOS catheter
*Ekos Catheter
Cindy Chan Follow Up Comment: Cards in PE management: The cardiologists have expressed willingness to assist with management of sub-massive and massive PEs, as many of them are credentialed to use the EKOS catheter.
- "On hours" 7a-7p: can call the on-call interventionalist for MASSIVE or SUB-MASSIVE PEs, as either they may be credentialed or should be able to get a partner who is help with this
- "OFF hours" 7p-7a: can call the on-call interventionalist for MASSIVE PEs to see if they are credentialed to assist; if not, then continue with our "traditional" course of management. SUB-MASSIVE PEs should be able to wait until the morning, when cards can be contacted if needed.
Iannitelli/Katiyar Oral Boards
Unfortunately I missed this excellent lecture.
PharmD Lecture Push Dose Pressors
Phenylepherine is the only drug at ACMC approved for bolus therapy. It is a pure alpha agonist with rapid onset and short half life.
Avoid phenylephrine in patients who are bradycardic. You could possibly cause worse reflex bradycardia.
ACMC Recommendation: 0.5-1ml (50-100mcg) of phenylephrine every 2-5 minutes. Can be used in the peri-intubation period and peri-code period.
Christine comment: Dopamine is universally available and is likely safer in an emergent situation. You and your nurses are less likely to make a dosing mistake with dopamine than with phenylephrine. The fail-safe way of giving emergent pressors is to just start a dopamine drip.
Mike Kennedy: Epinepherine could be used as a push dose pressor as well. PharmD response is that there is no data on using epi as a push dose pressor. It is not approved by our P&T Committee for push dose pressor use.
Elise comment: I don’t use push dose pressors. If I am resuscitating the patient in the peri-intubation period I will start a drip ofnorepi. The only time I use epi in a push dose situation is for anaphylaxis.
There was a discussion of what the ultimate aim of push dose pressors. You are just increasing BP transiently and not treating the underlying problem. On the other hand, there is a growing chorus in the EM world about using push dose pressors in the peri-intubation period for very unstable patients ie. “Resuscitation before intubation”. The patient oriented outcomes for this treatment will need to be studied further.
Urumov/Girzadas Recruiting Season Update
A. Patel Study Guide
Unfortunately I missed this excellent presentation.