Htet/Myers STEMI Conference
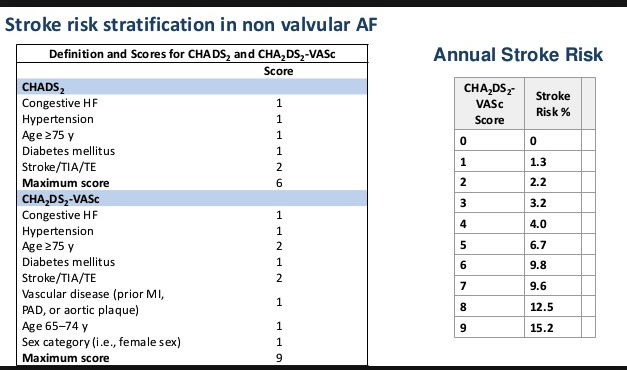
Case 1. 65yo female with Afib & RVR.
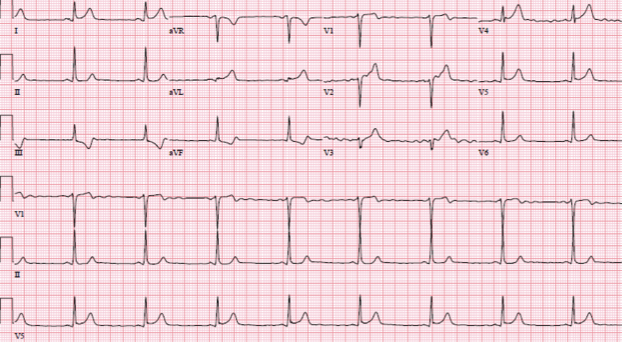
*EKG
*CHADS2Vasc Score for Stroke risk with Afib
* ACMC ED Afib Clinical Pathway
Dr. Silverman stated that chemical cardioversion of afib with ibutalide is preferred prior to electrical cardioversion because: 1. No sedation needed, 2. If Ibutilide fails, it does makes electrical cardioversion more likely to be successful.
Elise comment: Beware of hypomagnesemia when using ibutilide. Low mag can result in torsades when using ibutilide.
Case 2. 60 yo male presents with chest pain. Pt had prior coronary stent placement.
*EKG shows anterior q waves. Cath showed irregularity of LAD with no acute occlusion of stent.
Dr. Silverman comment: There is a new change to our STEMI protocol: The ED doc should ask the interventional cardiologist if they want an anti-platelet drug given in the ED. There are some new recommendations favoringBrilinta/Effient over Plavix. If Brilinta is given however, cardiac surgery is recommended to be delayed for 5 days. To keep it simple in the ED just give heparin and asa and ask the interventionalist whether they want Plavix, Brilinta, Effient, or no additional anti-platelet drug given . The P2Y12 anti-platelets are not time-sensitive and can be given in the cath lab.
Dr. Avula comment: No benefit to IV beta blockers in the ED.
Elise comment: Just to be clear we are
not routinely giving beta blockers in the ED. All the cardiologists agreed.
Risk of restenosis of a stent increases with 3 factors: DM, multiple stents, and small vessel lumen(<3mm).
Case3. 40 yo male with chest pain.
* EKG
Cath showed 100% LAD occlusion.
All cardiologists agreed this was a tough EKG to call a STEMI. Everyone felt bedside echo was useful in this case to identify focal wall abnormality. Also it was important to see that the EKG was evolving over minutes to an hour. Pericarditis does not evolve over minutes to an hour. Josh Eastvold/Jason Thomasello comment: Benign early repol does not have focal ST depression and the QTc will be less than 380. With STEMI’s, the QTc is usually >380. Early repol almost always has prominent R waves in V2-4. Pericarditis never has ST elevation in V1.
Follow up email from Elise: Dr. Silverman asked that we not give P2Y12 platelet inhibitors (Plavix, Brilinta, Effient) in the ED routinely for STEMI. There is not a time sensitivity to giving these agents in the ED as opposed to the cath lab, and Brilinta/Effient have received a higher level of recommendation in the latest iteration of AHA recommendations, so some cardiologists will prefer a different agent than Plavix. He will be discussing this with the interventionalists with the anticipation that these medications will routinely be given in the cath lab rather than in the ED. For now, it's reasonable to ask the interventionalist if they want Plavix or not, and please document if given.
Also, a reminder that the new Atrial Fibrillation pathway is active and on the Advocate website. It includes the option for Flecainide for chemical cardioversion of stable patients with Afib for < 24 hours of duration and no structural heart disease. (Flecainide + Structural heart disease = higher risk of bad dysrhythmias). Another alternative discussed this morning although not on pathway is Ibutilide. If using this agent be sure Mag and K are normal (Ibutilide + hypomag = Torsades).
Navarette M&M
60yo female with DM, HTN, CHF and smoking history. Patient presents with SOB and increased O2 requirement at home.
Exam showed 97% O2 sat on 4l. Patient has some lower extremity edema and scattered wheezing with diminished air movement bilaterally.
CXR shows infiltrate.
Initial treatment was nebs,steroids and antibiotics.
Patient had increased respiratory distress so team moved to intubate.
After intubation, BP drops to 60 and heart rate drops to 60 as well.
Re-evaluation of patient determined that auto-Peeping and air trapping in lung was the cause of patient’s rapid deterioration.
*Flow diagram of auto-Peep.
Strategies to counter Auto-Peep.
Increase the expiratory time by using an I:E ratio of 1:5
Decrease the respiratory rate
Use a tidal volume of 6ml/Kg
Sedate and Paralyze the patient
Use a large ET tube
Suction frequently
Use bronchodilators and steroids
Elevate the head of the bed
Chastain Study GuideEndocrinology
* Management of Thyroid Storm
* Management of Myxedema Coma. You also need to identify/treat the underlying cause such as infection or MI. Be careful giving thyroxine. IV thyroxine can cause an MI. Use small doses and give slowly.
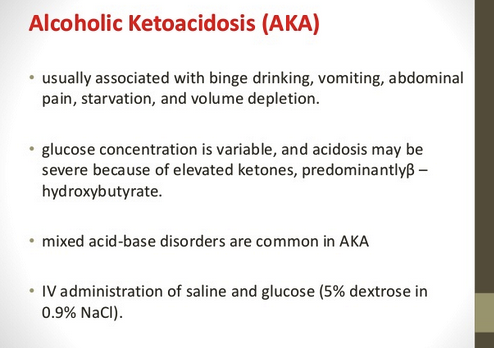
* AKA can have normal or only slightly elevated serum glucose levels.
*Adrenal Crisis Identification
* Adrenal Crisis Management
DKA management: no insulin bolus, no bicarb unless ph<6.9, no fluid bolus in kids unless they are in shock. Supplement potassium early on as long as patient is making urine. Activate the DKA protocol as soon as possible.
*Rule of 50 Glucose replacement for kids. Use D10 if child is <30 days old. D25 for kids 30 days to 2 years. D50 for kids 3 years and up.
Eastvold/Thomasello Lessons from the Community ED
Make sure you sedate patients adequately if you are going to use a neuromuscular blocker.
No need to rate control Afib with Cardizem if the rapid rate is due to fever or sepsis. Treat the sepsis and the rate will come down.
Don’t under-resuscitate the septic patient with a history of CHF or ESRD. Try to get as close to the 30ml/kg recommendation as possible. They can handle more fluid than you think.
When using insulin/glucose for hyperkalemia consider giving 2 amps of glucose and checking blood sugar on an hourly basis. There are many cases of hypoglycemia from this giving 10 units of insulin and 1 amp of glucose.
Kayexelate has no value for acute management of hyperkalemia. It takes hours to work and sorbitol by itself is similarly effective. Kayexelate has significant risks (intestinal necrosis, bowel perforation and concretions) Faculty in the room said they would still give it if nephrology advised it.
Strategies toimprove Press-Ganey scores: Look the patient in the eye. Shake the patient’s and family member’s hand. Sit down. Listen. Try to make 2-3 contacts with patient during their ED stay. The power of saying yes. (Avoid saying No directly to patient. Try to lower their expectations without using the word no. Say, “sure I will definitely try to do X but if we can’t, this will be our alternative plan.” )
Girzadas comment: Try to make a conscious note of the patient’s eye color. It is a mental strategy to spend enough time looking the patient in the eye.
Ways to calm a patient: Sit down, use calmest voice, and clarify any confusion. Don’t say "calm down", it doesn’t work. Feed the patient. Food is very effective in calming patients. If patient or family is upset, do a more thorough or protective work up. Ask the patient, “Did I do something to upset you?” Ask the patient, “What are you most worried about?”
Christine comment: If patients don’t like you, a more cautious work up may counter your internal bias against that person.
Nate West comment: Use the phrase, “We did extensive blood work today to evaluate your problem” (He learned this from Christian DenOuden)
If patients are very ill and you expect them to die, don’t sugar coat the prognosis to the family. Giving false hope may lead to blame down the line. Tell them, “the next 48 hours could be very rocky and you may want to call family to the hospital. Your family member is that sick.
Be alert for pyelonephritis with obstructing kidney stone. These patients get very sick very fast. Consider imaging the kidneys with bedside ultrasound in all urosepsis patients. Patients with pyelonephritis and an obstructing stone need emergent ureteral stent or urostomy tube placement.
Kelly comment: I have recently changed my practice to do a bedside renal ultrasound on all patients with pyelonephritis or urosepsis. I am looking for signs of hydronephrosis.
Eastvold comment: In any male with a UTI, you need to rule out 3 things: Ureteral stone, urinary retention, and prostatitis.
Be very concerned about pelvic fractures: Wrap the pelvis as soon as possible. Get blood/plasma started early. Transfer the patients to a Trauma Center if you are not at a Level 1 facility. If you are at the Trauma Center, look for free fluid in the belly with ultrasound. If free intra peritoneal fluid is present go to OR, if absent go to IR.
When intubating sick kids, just use ketamine. Don’t paralyze them. The acidotic pediatric patient can deteriorate so quickly that neuromuscular blocking increases your risk greatly.
Patients with trauma or sepsis who have transient hypotension with etomidate or pain meds are under-resuscitated. They need fluids/blood products and possibly pressors. Josh has observed that Tylenol in febrile septic patients can result in hypotension as their fever resolves. He won’t give Tylenol to febrile, septic patients until he has 2 liters of fluid on board.
PCARN guidelines do not apply to non-accidental trauma.