Barounis Engineering a better Cardiac Resuscitation
Organized practice on a regular basis can improve the function of the team during resuscitation. Dave spoke about optimal function of a resuscitation team based on practicing resuscitations, defining specific roles and locations for each member of the resuscitation team, and having a very organized and specific location for drugs and devices you may need in a resuscitation. It takes a lot of pre-planning and practice to have a great resuscitation team. It is very difficult to change hospital culture to accomplish this.
Physiology of Cardiac Arrest: There is a massive SIRS response when a patient has a cardiac arrest.
*Coronary Perfusion pressure is a key to getting ROSC. If CPP is <15 no arrested patient gets ROSC. IF CPP is >25 the patient usually will get ROSC. Pauses in chest compressions cause a drop in CPP. You have to really work on decreasing the number and length of pauses in compressions during ACLS care. Longer peri-defibrillation pauses of chest compressions have been show to result in higher mortality.
Mechanical chest compression devices have not shown a benefit over human chest compressions. Dave andEM faculty present at this lecture all felt the mechanical devices should be better than human compressions due to more consistent compressions and shorter pauses. Dave felt that all the studies using mechanical devices had relatively prolonged delays to defibrillation initially while medical personnel were applying the device. Erik also noted that centers that do these studies have outstanding quality of human CPR at baseline in the comparison group making it harder to demonstrate a difference. This level of quality of human chest compressions is really not reproducible in other medical centers.
Epinepherine is a double edged sword. It increases MAP and the likelihood of ROSCbut it also increases the risk of arrhythmia. Epi has alpha effect but also beta 1 effect. The beta 1 effect increases the arrhythmic risk. Electrophysiologists use esmolol to manage arrhythmias in the lab. There is a growing body of evidence for giving esmolol in patients in cardiac arrest who have failed multiple doses of epinephrine. Dave felt that if you have a patient who has failed defibrillation, amidarone, and 3 doses of epinephrine, it is reasonable to try esmolol. Elise asked if there is enough data on this concept to support an emergency physician giving esmolol during prolonged cardiac arrest. Dave felt it was reasonable to try 50 mg of esmolol in the patient who has failed the entire standard ACLS algorithm. Esmolol is used all the time in the electrophysiology lab and there are some papers supporting esmolol in cardiac arrest that has failed shock/epi x3/amiodarone. If you don’t get ROSC in 5 minutes after esmolol you can call the code. If you get ROSC, start an esmolol drip.
Bicarb doesn’t really help in cardiac arrest. It doesn’t change pH effectively.
Dave places an A-line in cardiac arrest patients to monitor their pulse and blood pressure. He feels it is way better than pulse checks. It picks up a pulse much better than palpation of the carotid and eliminates the pause in CPR for pulse checks. It allows you to better titrate pressors to elevate blood pressure to get CPP above 25. It also takes away “pseudo-PEA” where a pulse is present but you just can’t feel it. If you see an arterial wave form on the arterial line tracing you know you need added pressor effect to raise blood pressure.
Every cardiac arrest patient needs ETCO2 monitoring. If the ETCO2 jumps above 20 you have ROSC. Some people don’t even do pulse checks, they just watch for a jump in ETCO2.
Every cardiac arrest patient needs transthoracic echo to look for tamponade, pneumothorax or other causes of cardiac arrest. Dave says TEE in cardiac arrest is coming. Emergency medicine studies are already looking at this.
High dose epi did not have improved neurologic outcomes despite more frequent ROSC.
ECMO can save a patient if the patient had CPR started within 5 minutes of arrest. Patients with massive PE are the most optimal candidates. Dave advised consulting with CV surgery prior to giving TPA for massive PE to see if the patient can go to OR to be cannulated for ECMO.
*Double defibrillation with 2 defibrillator machines is something that can be tried if prolonged ACLS care with multiple defibrillations has failed. You applythe pads from two machines and defibrillate with both at the same time.
Regan/Kustad Oral Boards
Case 1. 76yo male with malaise, vomiting, and confusion. BP 104/76, febrile, other vitals OK. Exam demonstrated RUQ tenderness and mild jaundice. Imaging identified inflammatory changes around gall bladder. Diagnosis was ascending cholangitis. Treat with IV fluids and IV antibiotics. Consult GI for ERCP. Admit to ICU. Consult surgery.
*Acute Cholangitis (Slide from Dr. Ruby Wang)
Case 2. 40 yo female with severe pain in hand after exposure to rust remover containing hydrofluoric acid.
*Management options for HF acid exposure. If you are going to give intravascular calcium gluconate, give intra-arterial thru an A-line.
Case 3. 50 yo male presents with garlic odor. Patient has a lot of oral secretions. Lungs sound full of fluid. Patient had diarrhea in the bed. Patient ingested insecticide.
*Cholinergic Toxidrome
Critical actions: Hi dose of atropine. 2-Pam also should be given. The patient required intubation.
Kennedy
Ketamine is a very useful drug for multiple intubation scenarios. It doesn’t cause respiratory or CV depression. It is a bronchodilator. It also provides pain relief. It was once thought to be contra-indicated in patients with increased intracranial pressure. Now it is thought to be neuro-protective and indicated in patients with normal or increased intracranial pressure.
Etomidate works fast and is fast offset as well. It does cause respiratory depression. There can be some hypotension.
For procedural sedationKetofol (0.5mg/kg Ketamine mixed with 0.5mg/kg Propofol) This combination has fast onset, adequate length of sedation for most procedures and has less emergence phenomenon, less vomiting than ketamine alone, and less respiratory depression, and less hypotension than propofol alone.
Case scenarios: medication choice
Cardioversion: ketamine or propofol or ketofol.
Hip dislocation: ketofol
Pediatric forehead lac: Intranasal versed or intranasal fentanyl or both. There were conflicting views among the faculty on this one. Also give local anesthetic and po Tylenol.
Pediatric oral laceration: Ketamine. Harwood preferred Ketamine solo versus ketafol in this scenario.
70yo pneumonia who needs intubation: Etomidate and rocuronium
35 yo asthmatic requiring intubation: Ketamine for induction
22yo with status epilepticus: Ketamine and succinylcholine, however this scenario was also controversial
EMcrit reference: Although usually Rocuronium is the preferred paralytic, in status epilepticus succinylcholine may be preferable to allow determination of whether the seizure has been controlled. If Rocuronium is used, there is a risk that the patient may have ongoing seizure activity which is not observable, but which is nonetheless causing brain damage. Hyperkalemia secondary to rhabdomyolysis takes time to develop, so status epilepticus of short duration (<15-20 min) itself is not a contraindication to succinylcholine. For a patient who presents to the ED with seizure of unknown duration, Rocuronium is safer. Alternatively, this may be one situation in which sedative-only intubation may be a reasonable approach, as high-dose propofol will typically provide good intubation conditions provided that it breaks the seizure [more discussion about this below – see Addendum #2].
18yo altered trauma patient: Etomidate or ketamine. Ketamine these days may be preferred for neuro-protective effect.
50yo with FB in airway: Ketamine sedation with topical anesthetic. Pull out FB with a mcgill forceps.
Angioedema: Ketamine, topical anesthetic, no paralysis.
Marshalla/Ohl/Okubanjo Head & Neck Trauma
3 goals of management: Prevent secondary neurologic injury, identify treatable intracranial findings, identify other injuries.
*Epidural vs Subdural Hematomas
*DAI is due to axonal shearing caused by rapid deceleration injury.
*PCARN Head injury guideline for pediatric patients
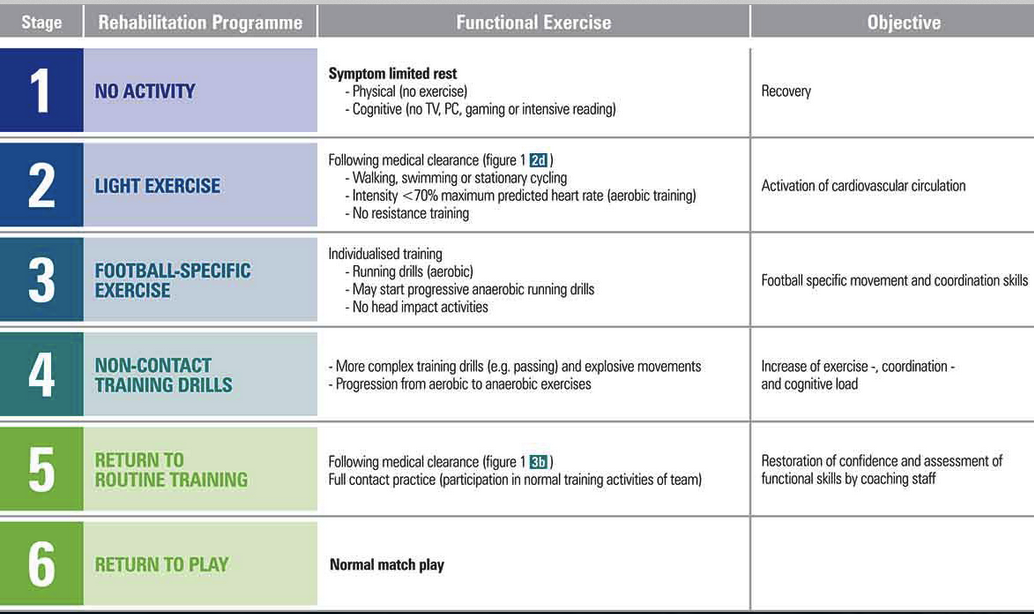
*Gradual “return to play” recommendations following concussion. The patient should not move to the next stage until they have been asymptomatic for at least one day at the current stage.
Lowering Intracranial Pressure: Either mannitol or hypertonic saline can be used. Dr. Lee (Trauma) prefers hypertonic because there is less risk of hypotension compared to mannitol.
*Neck triangles
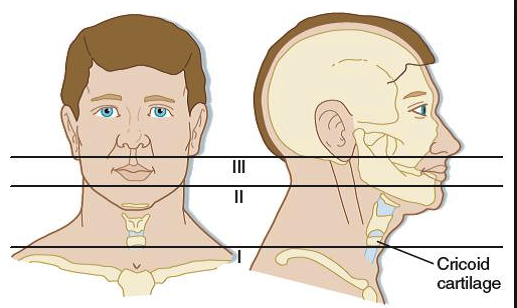
*Zones of the neck. Girzadas mnemonic: Zone 3 is close to the third ventricle and zone 1 is close to Big Red 1 (aorta).
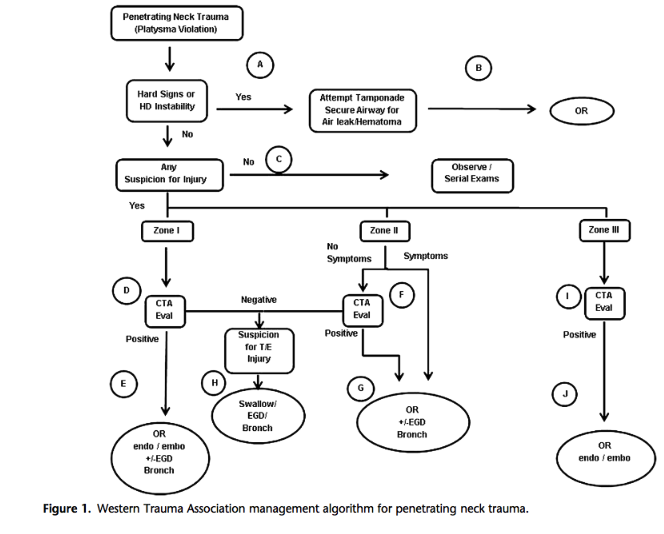
*Management guideline for penetrating neck trauma. Esophogeal injury is the leading cause of delayed death.
*Hard and soft signs of penetrating neck trauma
*NEXUS Criteria for C-spine Injury Harwood comment: NEXUS does not perform well in patients over age 65.
*Canadian C-spine Rule Elise comment: The Canadian C-spine rule scans all patients over age 65. It will also scan all patients with dangerous mechanism.