The patient then has a driveline that is connected to the rotor (located subdiaphragmatic), which exits the patient’s abdomen and connects to their battery pack.
Therefore since the LVAD is a continuous flow device, which unloads the left ventricle continuously, patients may or may not have a pulse.
The pulse is created by opening and closing of the aortic valve as it is directly related to their own intrinsic contractility. If you place an A-line you may see it be mostly flat with a MAP, hopefully, > 65. If a patient starts to regain cardiac function (myocarditis patients) then it is possible to have a strong pulse even with an LVAD. It is important to know that the aortic valve may not open in some patients, and that the patient’s hemodynamics don’t depend on it opening!
OK now that some of the basics are out of the way lets give some of the meat, what are the numbers on the device?
Pump speed (RPMs)
-This is how fast the rotor is moving usually somewhere between 8600-10,000 rpms. This is not picked arbitrarily. The RPMSs essentially is a major determinant of your cardiac output. SO some might say why not just go up higher on the RPMs if the patient is hypotensive? The answer is because the VAD is essentially a vacuum and if the cavity of the LV is too empty it may pull on the free wall or septum of the LV. These are called "suction events" which can precipitate dysrhythmias (have you ever put a guide wire in too deep and irritated the RV with frequent PVCs, try pulling on it with a vacuum).
The normal geometry of the LV should have the inflow cannula (going to rotor) facing the mitral valve without rightward or leftward shift of the septum or free wall.
If the patient becomes hypovolemic the LVAD may start precipitating suction events, because the RPMs are set too high for the relative amount of volume and pull on the septum. The VAD accommodates for these events by temporarily going down on the RPM's to try and reset itself.
PEARL: if the RPM's are changing on its own their it is likely a SUCTION EVENT, think hypovolemia or dysrhythmia.
RECAP: A ramp study (a study where someone “ramps up the RPMs” under echocardiography is required to change the RPMs because the geometry of the LV must be watched real time and therefore the RPMs should rarely be changed in the emergency department without an expereicned VAD provider doing so under echo guiadance.
The POWER (watts)
This is essentially how much power is required for the device to continue running at the set RPM's. There is no one number as it varies between patients and trending this number is usually the most helpful, the patients generally know where they have been running.
Why is the power important? The power and the RPMs are the only numbers on the VAD devices that are NOT GUESSTIMATES. All other numbers are derived from these two values.
If the power is increased it is because more work is required to continue turning the rotor at a fixed rate.
What could possibly cause the rotor to require more power to maintain the same set RPMs? Well the VAD is a synthetic device that is prone to clotting (about 1% incidence). If the INR is low, and you don't hear that nice hum of the VAD on auscultation, and instead hear a trapped weasel (I swear this is the closest thing I can imagine this as) maybe its a clot on the rotor. The machine is still trying to turn at constant RPMs but is pushing against a clot so more power is required.
Other causes of increased power are an increase in speed (RPMs) increase in volume status or an increased afterload.
What if the power is low, well you can imagine this means that the rotor is seeing less volume, this could be caused by hypovolemia or a CLOT either pre or post- cannula. A clot in the rotor will cause an increase in power, where as an LV thrombus or a thrombus on the outflow cannula will cause a drop in power.
Pump Flow (L/min)
The flow is a guesstimate of CO. Let me repeat that the FLOW is a guesstimate of the cardiac output. The flow depends upon volume status, LV contractility, the speed, RV function and afterload.
The heartmate II will alarm at low flow states < 2.5L/min and will show --- and flows that are above physiologic limits for a set RPMs just present as +++ on the LVAD.
Why is this important, well if there is a clot on the rotor, the machine has increased power, the same RPMs and the CALCULATED flow will be high even though the real flow will be far less. The machine knows this and gives you a clue to this by presenting +++ as a flow estimate since it is outside the physiologic range.
As mentioned before this is a flow estimate and is not analgous to cardiac output.
What is the Pulsatility Index? (dimensionless value)
Now things get really hairy. The flow is a calculated flow based on power and RPMs. And the PI is calculated from flow (max flow- min flow/avg flow over 15 seconds). So its calculated from a calculated number!
What it’s supposed to represent is the intrinsic contractilty of the LV. As the LV increases its contractility the flow will theoretically increase as more blood goes through the LVAD.
Joe Hsu my mentor puts it this way:
As the LV contracts, the flow through the pump increases due to an increased pressure at the pump inlet approximating the pressure at the outlet cannula (aortic pressure). During cardiac diastole, this inlet pressure drops, while the outlet pressure remains high (increased pressure difference) and, consequently, flow decreases. Therefore, pulse index is directly proportional to amount of LV contractility (increased due to preload, inotropic support, and myocardial recovery) and inversely proportional to the assistance provided by the pump.
So what you need to take from this is the PI estimates the amount of LV function, and as the patient becomes hypovolemic often times the PI will drop with their MAPs.
What are common LVAD complications?
1. Acute Anemia/Bleeding:
You have all seen this and is the most common reason patients with LVADs present to the ED, especially with GI bleeding. The question always comes up can you reverse the INR, and the answer is of course yes. If the patient has a significant bleed you should consider reversing it. They can bridge to heparin or integrilin in the ICU if need be when the patient is more stable. We do not start heparin for 5 days in fresh post-ops and a lot of times mid-ICU course they go unanticoagulated for days, and people don't clot off.
Hemolysis is another cause, which can cause significant anemia especially with a pump thrombus. LDH, haptoglobin, bilirubin as well as cell-free plasma hemoglobin can aid if you are very suspicious.
Can I give too much blood too quickly if they are end stage HF? Yes and NO the LV, sucks but that’s why they got the LVAD and as long as the RV is working please give the blood rapidly. If you notice RV failure (significant JVD, hepatomegaly, lower ext edema, assuming you don’t have a CVC for a CVP, which the CVP is not completely dead in this circumstance) then I would urge caution. Which brings us to
2. RV dysfunction:
This is a complication in about 20% of post-op patients and sometimes they have to crash onto an RVAD. This is badness. If the patient is not hypovolemic, and they are hypotensive and have signs of RV dysfunction you need a stat echo or do a bedside. Get an EKG are they ischemic, are they sub therapeutic in INR, did they throw a PE, is the LV so big its causing the septum to bow into the RV? do your best to figure out why is the RV failing.
Remember these were sick hearts to begin with, the LV gets fixed with an LVAD and then the RV sees all this additional flow it wasn't seeing before, and now a sluggish but getting by RV can become sick. If you have RV dysfunction you have got problems, and need a surgeons help quick. Thankfully this won't be common as most of these occur quickly after surgery.
How can you manage RV dysfunction, well a lot of times milrinone will aid in reducing pulmonary vascular resistance (PVR), and increases RV contractility. If you need to intubate do so cautiously as the PEEP from mechanical ventilation will worsen RV dysfunction and you should minimize hypoxia and hypercapnia as these two entities will worsen PVR.
If you suspect RV dysfunction get a VAD specialist in the ED immediately.
3. Infections:
These can be ugly, depending on where they are. These patients get blood cultures if they are febrile because they have a device, and will need long-term abx if infected. Replacing an LVAD is a morbid procedure and not one people are likely to do if they can avoid it.
Be a good doc and examine the abdomen and the site where the driveline comes out since it can be your source if its related to the LVAD (not a viral syndrome). These should get a CT scan to evaluate for an abscess if you don't find another otherwise obvious source (skin/ua/chest), and plain CT C/A/P usually will suffice. We usually start BROAD spectrum abx vanco and zosyn, and because of the device if the patient is in septic shock consider up front adding anti-fungal coverage with an echinocandin (micafungin, caspofungin or anadilafungin).
4. Tachydysrrthmias:
Ventricular arrhythmias
Why did they get the LVAD in the first place, ischemic cardiomyopathy is more likely to have irritable myocardium, but NICM is certainly entitled. These don't go away because they have an LVAD, and VTACH or VFIB can precipitate suction events as the RV may not be able to coordinate an adequate contraction which reduces LV preload. These dysrhythmias can be managed with cardioversion, which is not problematic, but can cause myocardial stunning afterwards. If they are stable VTACH consider amiodarone/procainimide or lidocaine and most of the patients have their own ICD's from their prior CM so make them comfortable if possible. If one of the first two doesn't work we usually add lidocaine as a bolus.
AFIB with RVR
Afib will also be problematic reducing RV function and therefore LV preload most surgeons here opt for rhythm control with amiodarone bolus and drip since they are anti-coagulated already with INRs 2-2.5.
5.Cardiac Arrest
Can I do chest compressions? Sure you can, but remember the LVAD is taking care of perfusion to the body so solving why its not doing that should be a priority. PE, hemorrhagic shock, RV failure, tamponade, hypovolemia etc…
The risks of doing chest compressions are dislodging the inflow and outflow cannula which if that occurs will likely result in massive exsanguination. So if you have to do it, you have to do it but take a second and try and figure out why the patient has coded. Otherwise continue with ACLS as per usual.
6.Aortic Insufficiency:
This adversely affects the pumps function by causing rapid LV filling and high pump flow as the outflow cannula is valveless and merely follows the path of least resistance (low pressure LV vs. higher pressure systemic vasculature).
Patients can present with left heart failure, pulmonary edema and hypoxemia. Treatment for mild AI is usually afterload reducing agents and diuretics, but for mod-severe AI may require a new valve or over-sewing completely of the original aortic valve in an effort to reduce the regurgitant jet.
BELOW is a TABLE of common complications and treatment options, its good reference in-case you need to look it up on a shift its courtesy of Joe Hsu, Critical Care at Stanford.
OK that’s a lot of information but it will get you started. Please e-mail me with questions and I’ll post-em on the site. If you have had a particularly challenging LVAD case let me know and if I don’t know the answer I have the mentors who will.
Talk soon!
-Dave
Table 1: Diagnosis and Management of Adverse Events and Complications
Complication
Clinical features
LVAD Parameters
Diagnosis
Management strategies
Diagnostic Studies
CT scan findings (7)
Inflow Cannula Complications
Kinking of inflow cannula
é Cardiac pulse pressure, Hypotension
ê Flow, power,
Variable flow
Coagulation parameters (INR 1.5-2.5), CT scan
--Kinking of inflow cannula
--Cannula malposition (Figure 6)
--Surgical consultation
--Anticoagulation
--Maintain adequate volume status
Thrombus in cannula
é Cardiac pulse pressure
Acute anemia (due to hemolysis), Hypotension
ê Flow, power
Evaluate for hemolysis: é cell-free plasma Hgb, indirect bilirubin, LDH; ê Haptoglobin
CT scan
--Low attenuation lesion in inflow/outflow cannula
--Surgical consultation
--Anticoagulation
Outflow Cannula Complications
Tearing of aortic anastomosis
Hypotension, Hemorrhage
No specific change
Serial Hgb, TEE, CT scan
--Extravasation of contrast material at anastomosis
-- Emergent surgical consultation
--Can occur over time
Kinking of outflow
Cannula
é Cardiac pulse pressure, Hypotension
ê Flow, power
Variable flow (positional)
Coagulation parameters (INR 1.5-2.5), CT scan
--Kinking of outflow cannula
--Disruption of cannula patency
--Surgical consultation
--Anticoagulation
Hemodynamic Complications
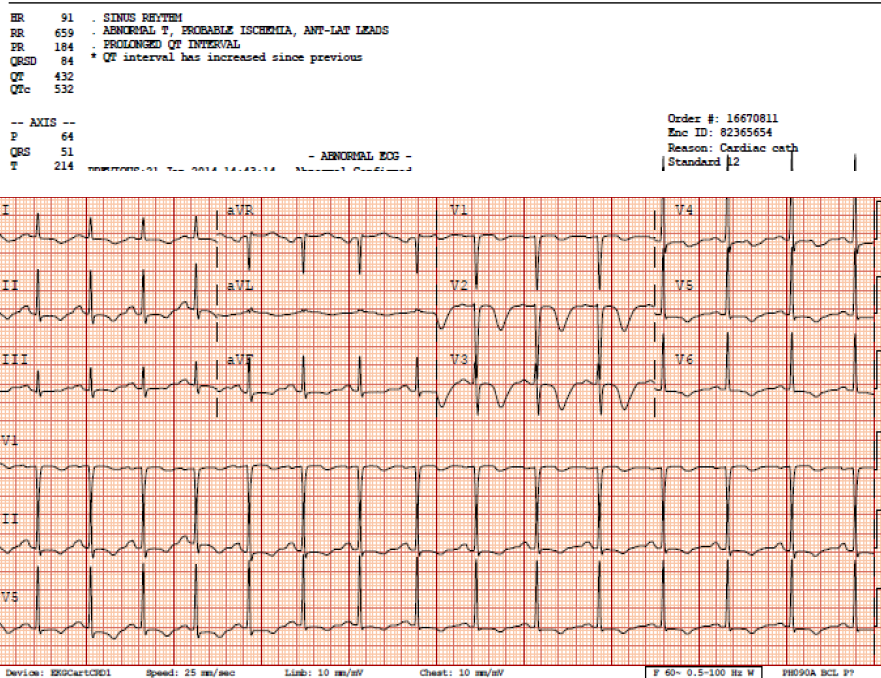
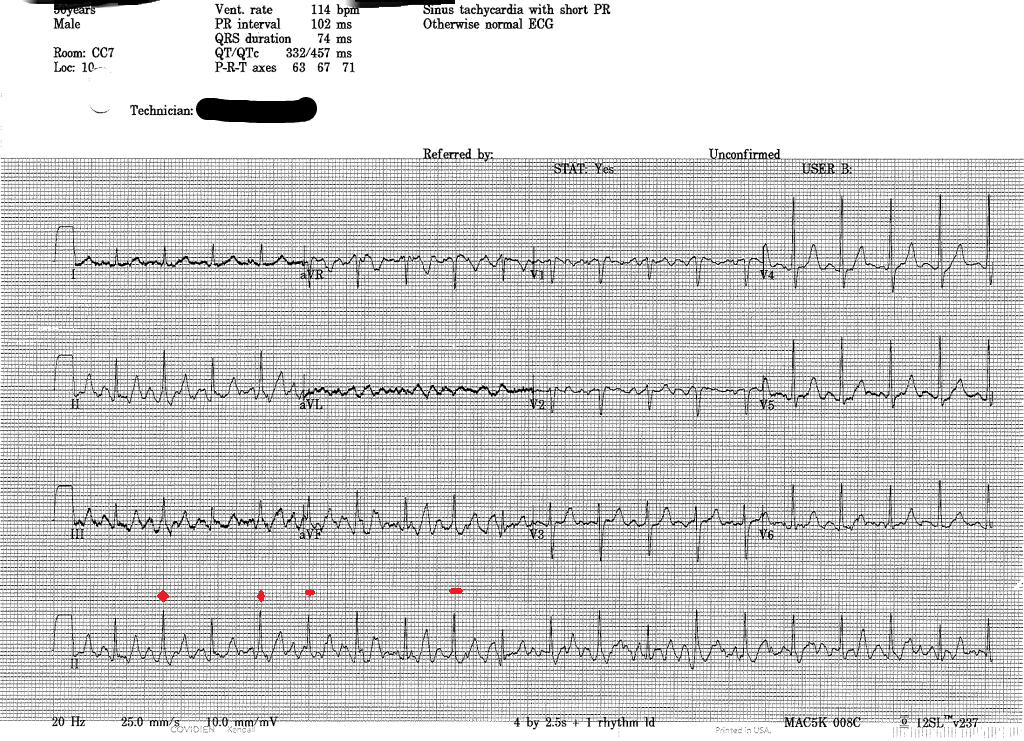
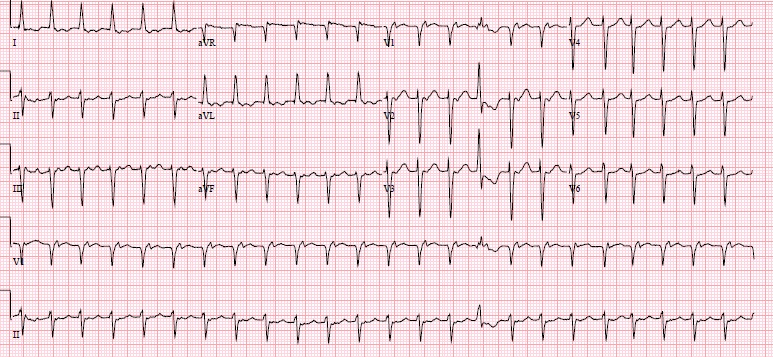
Arrhythmia
± Hemodynamic instability, Symptoms of ê perfusion
ê Flow, power
ECG, Electrolyte panel, TTE/TEE (to assess LV geometry, fluid status and cannula position)
None
--Control arrhythmia, defibrillation
--Evaluate for suction events-VT
--Watch for RVF
--External chest compression-onlyif in extremis
Right
Ventricular Failure
Hypotension, é CVP, PVR
ê Flow, power
Suction events
TTE, TEE, CT scan
CVC ± PAC
--Intraventricular septum bowed leftward,
--RV dilated,
--Dilation of IVC
--RV contractility: inotropes (Milrinone)
--Decrease PVR: avoid hypercapnia, hypoxemia, pulmonary vasodilators (iNO)
--Avoid overfilling
--Control arrhythmias
Pericardial tamponade
é CVP
Hypotension,
Preload dependent
ê Flow, power
Suction events
TTE, TEE (pericardial effusion may not be visualized on TTE), CT scan
--Dilation of IVC,
--Compression of right ventricle or atrium, flattening of heart border
--Pericardial effusion
--Pericardiocentesis
Aortic valve insufficiency
Decompensated heart failure, êSystemic perfusion, Cardiogenic shock
é High flow
TTE ramp study to evaluate speed, ECG-gated CT scan
--Presence of valvular thickening,
--Aortic valve visualized on ECG-gated CT scan
--May develop over time
--Consult cardiology and cardiac surgery
--Diuretics, afterload reduction
-- AI may improve with decreased pump speed
Coagulation-related complications
Thrombus on Rotor
Acute anemia (due to hemolysis)
é Cardiac pulse pressure
“+++” Flow,
éPower (>10-12 W)—hrs to days
Evaluate for hemolysis: é cell-free plasma Hgb, indirect bilirubin, LDH; ê Haptoglobin
CT scan
--Low attenuation lesion near inflow
--Surgical consultation
--Anticoagulation
Hemorrhage
Primarily GI also: Epistaxis, Hematuria, Mediastinal, Thoracic
ICH
ê Flow, power
Suction events
TTE, TEE, EGD, serial CBC, coagulation parameters, CT scan
Evaluate for acquired vWD: vWF antigen, vWF activity, factor VIII activity
Evaluate for hemolysis: é cell-free plasma Hgb, indirect bilirubin, LDH; ê Haptoglobin
--Evidence of bleed (e.g., ICH on CT head)
--PRBC and pro-coagulant factors as indicated
--Avoid excessive transfusions in:
-Bridge to transplant
-History of RVF
--?vWF replacement
Infectious Complications
LVAD-specific (41)
- · Pump/cannula infections
- · Pocket infections
- · Percutaneous driveline infections
LVAD-related (41)
- · Endocarditis
- · Bacteremia
- · Mediastinitis
Fever, Chills, Hypotension 2/2 sepsis,
Sequelae of embolic events
Variable effect on LVAD
CBC with differential, lactate
Exit site Wound Cx (+ Fungal Cx): if risk factors
TEE, if TTE negative
Blood Cx, if + CVC obtain “Time to positivity”Cx
Imaging: Ultrasound, CT (c/a/p)
--Gas or fluid collection around pump components, percutaneous lead
--Figure 4, pocket infection
--Figure 5, percutaneous lead infection
--Broad spectrum antimicrobials for nosocomial pathogens
± Fungal coverage based on risk factors
--EGDT
--Surgical consultation for incision and drainage, debridement, device exchange
Abbreviations: CVC: Central venous catheter, CVP: Central venous pressure, Cx: Culture, EGDT: Early goal directed therapy, GI: Gastrointestinal, Hgb: Hemoglobin, ICH: Intracranial hemorrhage, LDH: Lactate dehydrogenase, PAC: Pulmonary artery catheter, PVR: Pulmonary vascular resistance, RV: Right ventricle, RVF: Right ventricular failure, TEE: Transesophageal echocardiogram, TTE: Transthoracic echocardiogram, vWD: von Willebrand disease vWF: von Willebrand factor, W: Watts