Conference Notes 8-6-2013. A little late this week, but Another Great Day of Learning at Conference!
There are images in this document. If you don't see them, scroll to the bottom and click "View in Browser"
Please consider donating to our EM Foundation to benefit resident education/development. Thanks for your consideration/generosity.
/em-foundation/
Chastain U/S
I am sorry I missed this excellent lecture.
Campanella Code 30 (Acute Stroke)
Dizziness is a completely non-specific quasi-medical term and should be avoided. Try to get to a more specific term like vertigo, lightheaded, or ataxia.
New recommendation: The only labs you need prior to giving TPA for stroke is a finger stick glucose and an INR if the patient is on warfarin. The lower limit for glucose to give TPA is 50. Hypoglycemia below 50 is more likely to be the cause of neuro symptoms/findings than stroke. The upper limit of blood sugar is not defined. You can give TPA in the setting of hyperglycemia but also treat hyperglycemia with insulin.
Key HPI point is the last time patient was seen normal. That time starts the clock for the 3 hr or 4.5 hr windows for TPA.
Don’t delay CT scan for anything even physical exam, lab draws or xrays.
Dysarthria can result from multiple causes other than stroke. However, if someone is dysarthric, you should also worry about dysphagia. Must do swallow screening prior to oral intake in all stroke patients. Swallow screen is : If Aphasia is present then they should be npo. Next have them try sips of water, then drink a half cup of water. If they cough or struggle with these tests, then they should be npo.
Blood pressure control is another key management issue in stroke patients.
Door to CT scan completion time optimally should be 25min. Door to CT interpretation time should be 45min. Door to TPA administration time should be 60 min. Door to stroke unit time should be 3 hours.
Risk of serious hemorrhage (CNS or GI) from TPA is 6.5% and usually occurs within 48 hours. However, morbidity and mortality at 3months has been shown to be better than placebo.
If pt has signs of cortical stroke (hemi-neglect, visual field cut, global aphasia, dense hemiparesis) endovascular treatment may be indicated because likely there is a large vessel involved. Lovell comment: Can you comment on the negative outcomes in the endovascular trials in NEJM recently? Dr. Campanella said the findings are disappointing. He said they may not be valid because they used old technology. Campanella has seen many anecdotal successes. Lovell comment: What about all the patients who didn’t do well. Campanella: If patients have not improved with the standard of care TPA treatment then endovascular management may be indicated. The recent international stroke conference spent the majority of its time debating the use of endovascular results. Parker comment: The studies showed good reperfusion with the old device so why would new devices show benefit. Campanella response: There are mechanical differences between devices that may affect outcomes. Lovell: Future endovascular procedures should all be performed within the confines of an IRB approved study. Campanella: It is a problematic situation. Careful patient selection is critical for endovascular treatment of strokes.
Kelly Wiliamson comment: Would you ever activate a code stroke for suspected central vertigo? Campanella response: Without focality, no do not activate code stroke for vertigo. There is no category for vertigo on the NIH stroke scale. Harwood comment: Isolated aphasia with an overall low stroke score does uniformly well. Do you use TPA? Campanella: Depends on the severity of aphasia. Mild word finding problem does not warrant TPA but severe expressive aphasia does.
There are imaging modalities that can define the age of a stroke. There has been a study of “wake up strokes” (strokes first noted in morning when pt woke up) and they have found that the majority occur just prior to waking. Campanella has concerns about giving tpa for mild strokes. Difficult judgment calls.
Kettaneh/Girzadas Study Guide
Case 1 Infective Endocarditis. Critical actions: Get blood cultures (preferably 3) prior to antibiotics. Give IV antibiotic coverage for acute endocarditis (Vanc and Gent). Consult Cardiology and ID. Echo showed mitral vegetation. Mitral valve is the most common site to embolize. Pt had multiple signs of endocarditis (embolic phenomena, janeway lesions, osler nodes, glomerulonephritis, roth spots on fundi)
Case2 Iron poisoning in a pediatric patient. Critical Actions: IV Fluid Bolus, Serum Iron level, IV Deferoxamine. Optimal Care: Identify anion gap, Identify abnormal liver labs, Figure out history of iron overdose, Consult Toxicology/Poison Control, Admit to PICU. Serum Iron levels >500 are associated with serious toxicity. Pills but not liquid Iron may be visible on abdominal radiographs. Deferoxamine IV at 15-35mg/kg for 24 hours (ARDS is a potential complication). Classic presentation of severe overdose: Bloody diarrhea, Shock, Wide anion gap acidosis, Hepatic dysfunction, Leukocytosis, Lung Injury, hyperglycemia. Good mnemonic for anion gap acidosis: METAL ACID GAP Methanol/metformin/massive OD, Ethylene glycol, Toluene, AKA, Lactate, APAP, Cyanide/CO/colchicine, Iron/Isoniazid/Ibuprofen, DKA, Generalized seizure producing toxins, ASA, Paraldehyde/phenformin.
Case3 High Pressure Injection Injury. Critical Actions: Treat Pain, Identify High Pressure Injection Injury , Start IV Antibiotics, Consult Hand Surgeon for urgent surgical debridement. Optimal management: Get x-rays of hand, Update tetanus shot, Elevate affected hand, Keep Johnny NPO. High pressure injection injuries have 30% Amputation Rate. Amputation more likely if debridement is delayed >6 hours. Digital blocks are contraindicated. They can increase compartment pressure. Left index finger is most common location.
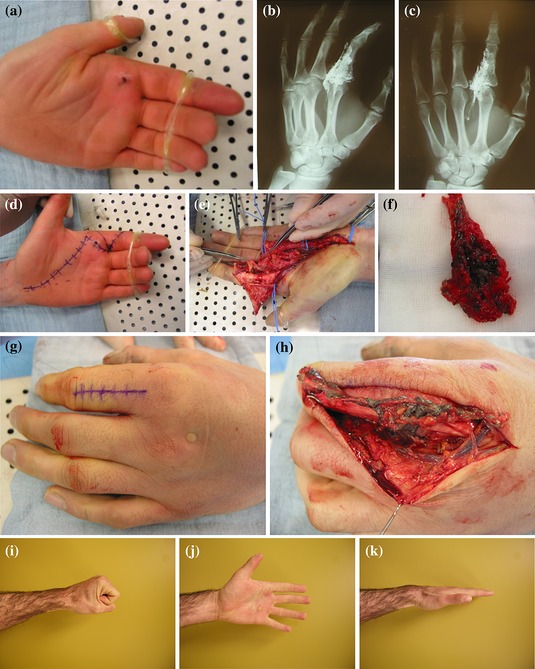
Google Image of Hi pressure injection injury and resultant surgical dissection.
Erickson Heat Emergencies
Prickly heat: Blockage of sweat pores leading to inflammation of sweat ducts. No specific treatment. Can use antihistamines or chlorhexadine lotion.
Heat cramps: Sweating leads to volume loss and hyponatremia resulting in cramping. Most commonly patients have been drinking hypotonic fluids. Treat with po Gatorade or IV NS.
Heat tetany: Hot environment stimulates hyperventilation leading to respiratory alkalosis and tetany of hands. Get patient to a cool environment.
Heat syncope: Variant of postural hypotension (volume depletion and vasodilation). Get to a cool environment and hydrate.
Heat Exhaustion: Due to dehydration and electrolyte depletion. Pt subjectively doesn’t feel right but still has normal mental status. Treat with rest in cool environment and IV or PO fluids/electrolyte repletion
Heat Stroke: True medical emergency. Classic heat stroke: Mostly affects elderly and chronically ill. Occurs in periods of high environmental heat stress. Exertional heat stroke: Healthy person who is exerting themselves in hot environment. Patients have altered mental status or seizures. Cerebellum is highly sensitive to heat and ataxia may be an early sign of heat stroke. LFT’s are usually elevated with heat stroke. Patients can get ATN and rabdomyolysis from heat stroke. Treatment of choice is evaporative cooling. Spray lukewarm water on skin and direct a fan at the patient. This is an effective cooling method pioneered in Mecca. You need to prevent shivering with benzo’s. Another effective cooling method is ice water immersion cooling. This is a method that is harder to perform. Another method is to use the device you use for therapeutic hypothermia (coolguard, arctic sun).
Girzadas comment: How do elite athletes complete the Badwater race (running 100+ miles through the desert) Brian Fort response: They drink specialized electrolyte drinks. Brian has drank a glass of liquid with 1400 calories and a ton of electrolytes. It tastes terrible.
Febbo Anaphylaxis
Diagnostic Criterion 1 — Acute onset of an illness (minutes to several hours) involving the skin, mucosal tissue, or both (eg, generalized hives, pruritus or flushing, swollen lips-tongue-uvula) and at least one of the following:
Respiratory compromise (eg, dyspnea, wheeze-bronchospasm, stridor, reduced peak expiratory flow, hypoxemia).
OR
- Reduced blood pressure (BP) or associated symptoms and signs of end-organ dysfunction (eg, hypotonia [collapse] syncope, incontinence).
Note: Skin symptoms and signs are present in up to 90 percent of anaphylactic episodes. This criterion will therefore frequently be helpful in making the diagnosis.
Criterion 2 — Two or more of the following that occur rapidly after exposure to a LIKELY allergen for that patient (minutes to several hours):
- Involvement of the skin-mucosal tissue (eg, generalized hives, itch-flush, swollen lips-tongue-uvula).
Respiratory compromise (eg, dyspnea, wheeze-bronchospasm, stridor, reduced peak expiratory flow, hypoxemia).
- Reduced BP or associated symptoms and signs (eg, hypotonia [collapse], syncope, incontinence).
- Persistent gastrointestinal symptoms and signs (eg, crampy abdominal pain, vomiting).
Note: Skin symptoms or signs are absent or unrecognized in up to 20 percent of anaphylactic episodes. Criterion 2 incorporates symptoms and signs in other organ systems and is applied to patients with exposure to a substance that is a likely allergen for them.
Criterion 3 — Reduced BP after exposure to a KNOWN allergen for that patient (minutes to several hours):
- Reduced BP in adults is defined as a systolic BP of less than 90 mmHg or greater than 30 percent decrease from that person's baseline (Up to Date)
Skin/mucosal findings can be absent 10% of the time. Respiratory signs are present in up to 70% of patients. GI signs are present in 45% of patients and can be a sign of impending cardiovascular collapse.
PCN and NSAID’s are the two most common drugs causing anaphylaxis.
Immunologic (anaphylactic)and non-immunologic reactions (anaphylactoid)are treated in an identical manner.
Mechanism of shock is vasodilation, fluid shifts and myocardial depression.
Anaphylaxis onset is within 30 minutes of exposure.
80% of reactions are uniphasic. Biphasic reactions most commonly occur within 10 hours but can occur out to 72 hours.
Treatment: Epinepherine/IV fluids/Airway management. No contraindications to epi in the setting of anaphylaxis. Just use IM Epipen or Epipen jr (kids <30kg). No need to remember the dose of epi just use the epi pen.
Harwood comment: You have to leave the epipen in the muscle for 5-10 seconds to allow it to auto-inject. Elise comment: I was in the PED recently and the nurse pulled the epipen out right after sticking it in the muscle. We had to administer a second epipen and make sure it was in the muscle for 5-10 seconds.
Empty ventricle syndrome : Pt’s treated for anaphylactic shock in the ED who get up to walk to bathroom while they are still vasodilated and tachycardic develop an empty ventricle and go into PEA. There are case reports of this. Brian recommended keeping pt’s supine for 30-60 minutes after treatment for anaphylaxis.
Anaphylactic shock should be treated with iv epi. Criteria is marked hypotension or patient is still symptomatic after two IM epipen injections. Give infusion of epi : 1mg in 1 liter of saline and infuse at 2ml/min. Nick Kettaneh comment: http://academiclifeinem.com/dirtyepi/ describes the making of this drip. This reference says you can run the drip wide open. Each ml of this drip has 1 microgram of epi. Girzadas advice: probably start drip somewhere between 2-10 ml per minute and titrate up if needed. Bolus dosing not recommended. Vasopressin is probably best choice for refractory shock if epi fails.
Adjuvant therapy: Steroids, diphenhydramine or zyrtec (second generation antihistamines are effective and less sedating), ranitidine or pepcid, albuterol or racemic epi nebs for wheezing. Glucagon is indicated if patient is on a beta blocker. Everyone gets a 6 hour observation. Selected patients should be observed for 24 hours (severe symptoms, hx of asthma, use of betablockers, extremes of age, barriers to care)
Give everyone a referral to an allergist.
Bradykinin induced angioedema: ACE-I and Hereditary angioedema. HAE may have intense abdominal pain and can mimic a surgical abdomen. Treat HAE with FFP. Ecallantide and Icatibant are new drugs for this disease but we don’t have them at ACMC.
ACE-I angioedema: Lip edema rarely progresses to involve the airway. Edema of tongue/soft palate/larynx have higher risk of needing airway intervention.
