Here's to the start of another outstanding academic year! Welcome to all the new ACMC EM Interns!
Beckemeyer/Girzadas Oral Boards
Case1. 30 yo pregnant female presented after MVC. Patient had hypotension, abdominal pain/cramping and vaginal bleeding. FAST showed no intra-peritoneal blood and the fetus was bradycardic. Traumatic Placental Abruption with associated DIC was the diagnosis. Critical actions were to place patient in left lateral decubitus position to off-load the IVC, resuscitation with blood products and fluids, consult OB to perform emergent c-section. One learning point was that in this situation it would be prudent to activate the massive transfusion policy. These patients may require large quantities of PRBC’s, platelets, FFP and cryoprecipitate. Another key point is that ultrasound is insensitive for diagnosing placental abruption. However, if ultrasound is positive for abruption, it is very specific. In the stable patient, fetal monitoring has a higher sensitivity for picking up abruption.
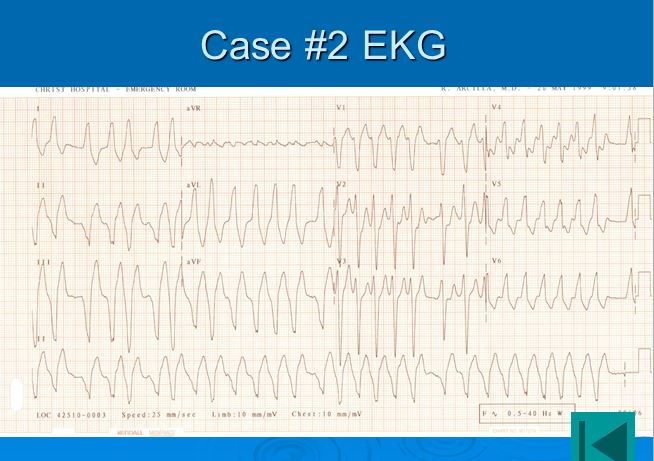
Case2. 40 yo male presents with palpitations and rapid heart rate. EKG showed an irregular rhythm with both wide and narrow complexes.
Diagnosis was AFIB with WPW aberrant conduction.
Critical actions: attempt chemical cardioversion with procainamide (preferred choice), ibutilide, or amiodarone. When the patient decompensated and became hypotensive, proceed to electrical cardioversion. Harwood made the point that Afib can be resistant to electrical cardioversion so it was prudent to perform cardioversion at an initially high dose like 150-200J.
Case3. 6 yo female with gross deformity of her left elbow after falling from her bike. Xrays showed a Gartland 3 supracondylar fracture. Critical actions were to treat pain, perform a careful NV exam, and arrange urgent/emergent surgery. There was general agreement among the faculty that they would not attempt closed reduction of a displaced supracondylar fracture unless the neurovascular status of the affected limb was severely impaired and there was going to be a significant delay to get the patient to the OR. If the patient has a diminished radial pulse, check for warmth of fingers, cap refill, pulse ox wave form of fingers of affected extremity, and doppler the radial pulse. If any of these are present and you can get the patient to surgery within 2-4 hours just keep patient in the position of comfort and no need for the emergency physician to attempt closed reduction.

Lovell/Urumov/C. Kulstad How to Give a Good Lecure
First tip: To give a more engaging lecture minimize your use of power point. Try to think of non-powerpoint methods to interact with the audience.
Be sure you have your technology pre-tested, and make sure it is working before you try to use it during a presentation.
Elise gave a “bad presentation” example and the audience made the following comments: You need to have good contrast between fonts/background on your slides. Spell check your slides. Get out from the podium to interact with the audience. Change up your intonation and pace of speech to keep the audience engaged. Limit your slides to 6 lines with only 6 words in each line. More than that is too much. Reading your slides verbatim is the marker of not being prepared/putting the talk together at the last minute.
The audience is only capable of picking up 3 key points from any lecture. So hammer home those points.
Elise’s “good talk” example was given next: Talk had an exciting title that immediately hooked the audience. She asked the audience questions. Each topic started with a relevant case example. She gave focused learning points. The lecture points were very EM clinically oriented. She hammered home the key points repeatedly. More useful diagrams on her slides. Slides had no more than 6 lines with 6 or less words in each line. She knew her audience and really presented the topic in an EM relevant way. She wrapped up the talk with a nice summary/wrap-up/repeat of the key points. Harwood comment: Powerpoint is not all bad. It helps you organize your topic. It allows you to use pictures and videos and give info in a concise way. The key is to be interactive when using powerpoint.
Andrej’s “bad talk”: Audience comment: Anrdrej was apologizing for his talk. Multiple spelling errors on his slide. Too much data on a slide. He had a phone call interruption during his talk. He was very non-specific in his learning points. Poorly developed explanations of the information on his slides. He started reading his slides facing away from his audience and toward the screen. Impossible to read his slides due to lack of contrast. Unappealing slides. Distracting transitions. Weak opening. Self-undercutting of his authority. Playing with coins in his topic was very distracting.
Iannitelli comment: About 10% of the population is color bind so black/white and blue/yellow or blue/white are better than most other colors.
Andrej’s “good talk”: Much more interesting title. Slide colors were very good. He engaged the audience and asked them questions and examples. Kept slides to six lines with no more than 6 words per line. Graphs and charts were much more clear and he explained them with much more clarity.
Christine’s “bad talk”: Too much info on the slides. Pictures on the slides were very small. She was shifting back and forth constantly while facing the screen. She frequently contradicted herself while speaking. There were misspellings on the slide. Her video link did not work.
Christine’s “good talk”: Much more interesting title. Pictures larger and more pertinent to her presentation. Much fewer words on each slide. She faced the audience while speaking. Not constantly shifting back and forth. The explanation of each slide was much more clear. The intonation and pace of her speech was much more varied and effective.
Elise comment: Always finish your talk early to be respectful of peoples’ time.
Beckemeyer and Permar Resuscitation of the Critically Ill/Cardiac Arrest Patient
The ABCDEF's of critical thinking during a resuscitation.
A=Aorta and acidosis. Always consider these two entities as causes of shock.
B=Bagging and Baby on Board. Avoid hyperventilating patients and always consider that a female may be pregnant
C=Compressions and Cooling. Push hard and fast for CPR and Cool the patient when you get ROSC.
D= Defibrillation/CPR push hard and push fast/Cool the patient if you get ROSC. Keep compressions going when you are charging the defibrillator. There is some debate about the safety of compressions during defibrillation. Harwood comment: it is probably safe. Erik comment: there is no way for the person doing compressions to sustain a shock from the defibrillator.
D=Drugs/Dextrose Consider overdose and hypoglycemia in the altered critically ill patient. Multiple attendings said they had intubated patients who were later found to be hypoglycemic.
D=DOPES mnemonic for ventilation/oxygenation problems with ventilator. Dislodgement/Obstruction/Pneumothorax/Equipment failure/Stacking breaths in COPD/Asthma
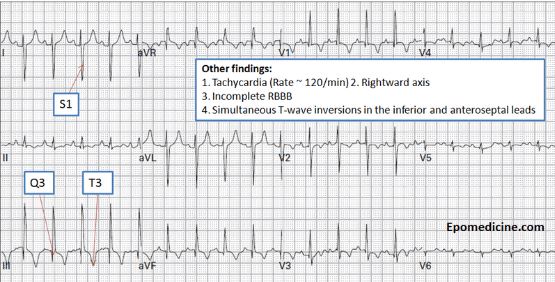
E=Effusion and Embolus Pericardial effusion can look clinically like a PE. Do an echo before you start treating PE. The treatment for these two diseases is markedly different. Electrical alternans is classically associated with pericardial effusion. Echo can be helpful identifying both diseases. EKG in PE can show S1Q3T3 and/or t wave inversion inferiorly and anteriorly.
If BP improves markedly with intubation consider the diagnosis of PE. Positive pressure ventilation improves the hemodynamics of the PE patient.
F=Forget about it. These don’t work for resuscitation: Bicarb, mag, lidocaine, and atropine. Lidocaine and defasiculating meds for RSI. Trandelenburg positioning.
LVAD Team Care of the LVAD Patient
Most patients would survive for awhile if the LVAD battery power ran out. Some would die in a few minutes.
All patient who get an LVAD have an EF <25%. They are all in class 3-4 heart failure.
LVAD has been shown to improve quality of life and survival. The LVAD team has a patient who is still working as an anesthesiologist with an LVAD!
All VAD’s have the same 4 components: 1. Inflow cannula in the apex of left ventricle pointing at the mitral valve. 2. Mechanical pump. 3. Outflow cannula to the aorta. 4. Drive line. The drive line is connected to a controller. The LVAD team has seen multiple patients present through the ED with a disconnected drive line. This simple problem can prove to be fatal.
If a patient presents with critically low battery power. Call SHU or 9E/W to get extra batteries brought down.
Everyone in the audience was given the opportunity to connect/disconnect the drive line and battery packs to practice. If a patient is in the ER with a disconnected drive line or battery, these need to be re-connected ASAP. Some patients have died due to a disconnected drive line.
There should be a VAD Coordinator in the hospital from 7a to 7p. If they are not physically present in the ED they are available by phone. ASHU is another resource to contact if you have any difficulty getting a VAD Coordinator.
Resucitation: Chest compressions are indicated during resuscitation if the pump is not working (If the pump is not working, it will be alarming). If the pump is working and not alarming, you don’t need to do CPR because the pump is working.
It is thought that good chest compressions prevent clotting of an LVAD with pump failure. Defibrillation is OK for V-fib. Never disconnect patient from LVAD equipment. If the pump is not working it is ok to give milrinone to increase contractility. It is ok to give levophed for hypotension.
If AICD is firing, get the AICD interrogated. There is a phenomenon of “phantom shocks” in patients who have been shocked multiple times in the past. Consult the EP cardiologist. The LVAD team fixes the plumbing (LVAD) but doesn’t deal with the electricity (AICD). The most common problem causing AICD firing is hypovolemia. Dehydration from the flu is enough to cause hypovolemia and AICD firing.
Depending on how high the flow rate is set on the LVAD, a patient may or may not have a pulse. Accurate measurement of BP is only possible via an A-line in a patient with no pulse. You may be able to hear a single kortokof sound when taking a brachial bood pressure using a Doppler. In a pulseless patient that sound corresponds most likely to a mean arterial pressure. In a patient with a pulse the kortofkoff sound corresponds to a systolic pressure.
It is ok to give cautious fluids to a patient you think is hypovolemic. Echo may be helpful to determine if a patient is hypovolemic. You may see LV collapse due to the pump sucking all the blood out of the under-filled LV.
If the VAD is not alarming, the VAD is working. In an altered patient with a non-alarming LVAD, the patient’s altered mental status is likely due to a non-VAD cause.
Elise comment: In a hypotensive LVAD patient that does not have a pump alarm going off you have got to look for non-VAD causes. LVAD team response: Get CT head for stroke, check their HGB (significant anemia for these patients is around 7-8), do a rectal exam for GI bleeding, look for sepsis, check an LDH and peripheral smear for hemolysis.
There is one case of pump failure that won’t cause the pump to alarm and that is a clotted pump. The pump doesn’t alarm because it is still running. However it can’t pump clotted blood. These patients will present with chest pain, SOB, acute heart failure, and hemolysis (LDH > 1000). These patients need to go to the OR immediately for a new pump.
Best central line approach in the LVAD patient is a Right IJ.