Joint EM-Peds Conference on Complications of Sinusitis
Don't treat sinusitis unless the patient has fever 102+ with 3-4 days of green/yellow drainage OR their symptoms have lasted more than 10 days or they have worsening symptoms after initially improving.
If a patient has headache, or mental status changes or forehead swelling associated with sinusitis. You need to suspect intracranial involvement such as pott's puffy tumor. The diagnostic test of choice is a CT head with contrast. A plain CT will miss significant diagnoses. Harwood comment: You can order a CT head with thin cuts through the sinuses to optimize your view of the sinuses.
The cases presented with complications of sinustis described children with many days of sinusitis symptoms with associated fever and headaches. If kids have headache or mental status changes associated with fever and sinusitis get a contrast ct head with fine cuts through the sinuses.
Typical appearance of Pott's Puffy Tumor
Pott's puffy tumor with brain involvement.
Treat sinusitis with antibiotics and nasal steroids to attempt to prevent complications of sinusitis. Dr. Collins made the point that 50% of sinusitis treatment is nasal hygiene with nasal steroids. Dr. Sherman also stated that saline nasal spray and clearing nose with blowing is important as well.
If a child has swelling of the forehead, be very cautious chalking it up to a bug bite. The children presented at this conference had bumps on the forehead diagnosed as bug bites that turned out to be pott's puffy tumor.
Dr. Collins comment: Strep anginosis is sub-type of strep viridans. It is known to cause complications of sinusitis especially abscess. If you have a child with a positive blood culture or other culture for strep anginosis, you have to look very carefully for abscess including intracranial abscess.
Harwood comment: If I see any meningeal involvement on a contrast ct with sinus disease, that patient is going to the ICU and needs ID, ENT and Neurosurgery consults.
Staley Study Guide Pediatrics
Most common causes of pneumonia in children with cystic fibrosis is staph aureus and H. flu.
If you are giving a prostaglandin infusion in a neonate to re-open the ductus be on guard for apnea. Apnea and flushing are side effects of prostaglandin infusions. If you have to transfer a patient receiving prostaglandins it is recommend to strongly consider intubation prior to transfer in case the child becomes apneic during transfer.
Shock or cyanosis in the first 2 weeks of life should raise the suspicion for congenital heart disease as the ductus is closing during this time period.
Components of Tetrology of Fallot
Knee-Chest position to treat a Tet Spell. Also give oxygen, IV hydrate, and give morphine 0.1 mg/kg. By then you should be consulting Peds Cards or PICU. But other strategies that can used are ketamine, phenylepherine, and esmolol.
Young infants with vomiting and or diarrhea have a high risk of hypoglycemia. Check a dexi. After initital boluses, give glucose containing maintenance fluids in kids.
If a child under 1 yo has bilious emesis you need to work up that patient with an upper GI for suspected malrotation with midgut volvulus. There may be an emerging role for ultrasound to screen for this disease process but you can't rely on ultrasound yet. Harwood comment: If you can't get an upper GI done in a rapid fashion at your institution you need to transfer to a pediatric center.
Classic "corkscrew sign" of Midgut Volvulus on Upper GI
Shimanuki et al [8] evaluated the clockwise “whirlpool sign” by color Doppler ultrasound in diagnosing midgut volvulus. In 13 patients with surgically confirmed midgut volvulus, color Doppler ultrasound showed clockwise “whirlpool sign” in 12 patients and no “whirlpool sign” in one patient. The sensitivity, specificity, and positive predictive value of clockwise “whirlpool sign” for midgut volvulus were 92%, 100%, and 100%, respectively [8].
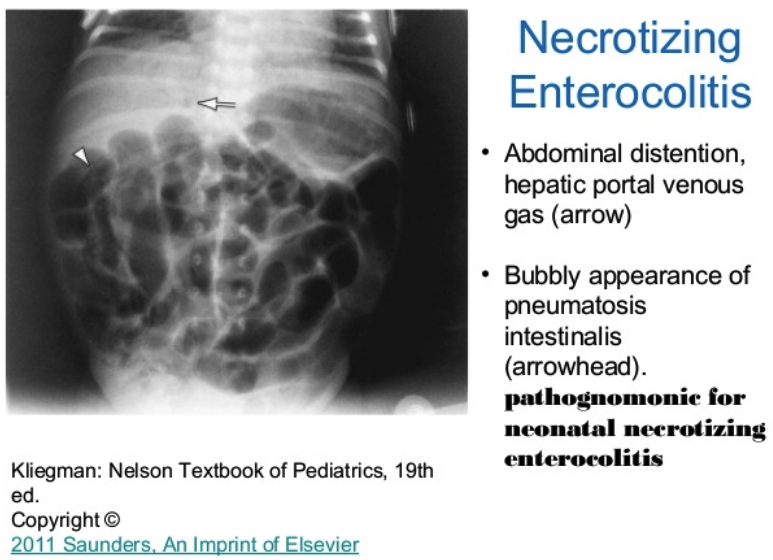
Clinical signs of NEC
When considering NEC, on xray look for portal gas and pneumatosis intestinalis.
Destefani M&M
When dealing with a sick patient, be sure to communicate with the family clearly and prognosticate the possibility of death or poor outcome. It is better to prepare the family for this possibility early on in the ED course.
When you have to give bad news, focus all your attention on that family. You owe it to that family to not have distractions during that time. Speak to the family in a quiet place. Turn off your phone. Wear your coat. Know the patient's name and check with the family that they are here for that patient. Give the family an appropriate amount of your time. Shake everyone's hand. Sit down, lean forward. Have security officer nearby if you think there is a possible safety risk. Make eye contact, speak slowly and clearly. Use the word "died". Allow a 10 second pause after breaking the bad news. Then express your sympathy and availability for the family should they have any questions. Kelly Williamson comment: Reassure the family that they did everything right and they did the best they possibly could to care for the patient leading up to this event. If you have to use a translator during bad news, be sure to contact the translator and prep them prior to walking in to meet the family.
Pick one case every shift that you felt didn't go as well as possible. On your way home from the shift consider what went well and what didn't go well. Think about what you would have done differently and how you would act differently the next time.
Katiyar Billing and Coding Medical Decision Making
Include in your medical decision making any medications the patient may be taking that are relative to this ED visit. Also include the medications you used to treat the patient in the ED.
Document your Differential Diagnosis.
Document that you discussed the case with the patient and or the family.
Document patient re-evals.
Include your interpretation of prehospital ekgs and rhythm strips.
In your medical decision making, include any guidelines such as PERC , Well's, PECARN, or Heart Score that you used to guide management.
In general terms, when document your MDM, describe the patient, describe what you did for the patient, describe what you ruled out, what is the most likley diagnosis, and describe your disposition of the patient.
www.Ritecode.com Jeffrey Restuccio, CPC, CPC-H jeff@ritecode.com
www.Ritecode.com Jeffrey Restuccio, CPC, CPC-H jeff@ritecode.com










![Shimanuki et al [8] evaluated the clockwise “whirlpool sign” by color Doppler ultrasound in diagnosing midgut volvulus. In 13 patients with surgically confirmed midgut volvulus, color Doppler ultrasound showed clockwise “whirlpool sign” in 12 patien…](https://images.squarespace-cdn.com/content/v1/55d5e97fe4b0c4913b06a4dd/1511367591796-HLSB2K15X45NLDXH8LJA/Snip20171122_10.png)